Published online Jun 28, 2007. doi: 10.3748/wjg.v13.i24.3279
Revised: February 3, 2007
Accepted: February 8, 2007
Published online: June 28, 2007
The investigation of small bowel morphology is often mandatory in many patients with Crohn’s disease. Traditional radiological techniques (small bowel enteroclysis and small bowel follow-through) have long been the only suitable methods for this purpose. In recent years, several alternative imaging techniques have been proposed. To review the most recent advances in imaging studies of the small bowel, with particular reference to their possible application in Crohn’s disease, we conducted a complete review of the most important studies in which traditional and newer imaging methods were performed and compared in patients with Crohn’s disease. Several radiological and endoscopic techniques are now available for the study of the small bowel; each of them is characterized by a distinct profile of favourable and unfavourable features. In some cases, they may also be used as complementary rather than alternative techniques. In everyday practice, the choice of the technique to be used stands upon its availability and a careful evaluation of diagnostic accuracy, clinical usefulness, safety and cost. The recent development of innovative imaging techniques has opened a new and exciting area in the exploration of the small bowel in Crohn’s disease patients.
- Citation: Saibeni S, Rondonotti E, Iozzelli A, Spina L, Tontini GE, Cavallaro F, Ciscato C, de Franchis R, Sardanelli F, Vecchi M. Imaging of the small bowel in Crohn's disease: A review of old and new techniques. World J Gastroenterol 2007; 13(24): 3279-3287
- URL: https://www.wjgnet.com/1007-9327/full/v13/i24/3279.htm
- DOI: https://dx.doi.org/10.3748/wjg.v13.i24.3279
The small bowel has been defined for many years as the “black box” of the gastrointestinal system due to its inaccessibility to endoscopic exploration. Indeed, until recently, the only available endoscopic technique to explore the small bowel, the so-called push enteroscopy, was very seldom able of a complete small bowel exploration; this may become an important limit, particularly in Crohn’s disease which often involves the most distal portion of the ileum[1].
Therefore, the conventional radiological methods, i.e. small bowel enteroclysis (SBE) and small bowel follow-through (SBFT), have long been the only imaging methods providing information on the morphological features of the small bowel valuable in the diagnosis and management of Crohn’s disease.
In the last few years, several alternative techniques have been proposed for imaging of the small bowel. Indeed, the evaluation of bowel wall features, as well as of extra-intestinal involvement by bowel ultrasound (US), has gained diffuse popularity. At the same time, developments in hardware and software components, as well as in the use of contrast media, have led Magnetic Resonance (MR) and Computed Tomography (CT) to have a recognized role in the study of intestinal diseases and of their intra-abdominal complications.
Furthermore, recently the direct visualization of the mucosa of the whole small bowel has become possible thanks to the development of video-capsule endoscopy (VCE) and of “double-balloon” enteroscopy.
The aim of this review is to point out the most recent advances and the advantages and limitations of the various imaging techniques now available for the study of the small bowel, with particular reference to their use in patients with suspected or proven Crohn’s disease.
As stated before, investigation of the small bowel in Crohn’s disease has been based for a long time on radiological techniques, such as small bowel enteroclysis (SBE) and small bowel follow-through (SBFT).
Typical small bowel changes which can be observed by means of these techniques include irregular thickening and distortion of the valvulae conniventes, loops adhesions (mass-like effect) or separated loops because of wall thickening and mesenteric inflammatory infiltration. Transverse and longitudinal distribution of ulcerations can separate islands of thickened internal wall, resulting in the typical cobblestone appearance. Strictures are often separated by healthy bowel tracts (skip lesions); impaired small bowel peristalsis is commonly observed within rigid stenotic tracts. Extrinsic compression may be observed, due to mesentery lymph node enlargement[2,3].
The conventional technique was historically able to differentiate between Crohn’s disease, granulomatous enteritis and ulcerative colitis[2,3].
Both SBE and SBFT, when performed by experienced examiners, appear to be characterized by similar sensitivity (85%-95%) and specificity (89%-94%) in detecting the radiological lesions typical of Crohn’s disease. The preference for one technique or the other largely depends on institutional standards[4,5] while the preference of patients is usually in favour of SBFT since no nasal (or oral) intubation is required. SBFT is also usually associated with a lower radiation exposure and is a less expensive and time consuming examination; moreover, SBFT does not miss duodenal disease[6].
Both procedures are able to evaluate small bowel peristalsis, the intra-abdominal distribution of bowel loops, the presence of strictures and dilatations, the distensibility of the intestinal lumen, the presence of fistulae (Figure 1), the morphology of circular folds and other features of the mucosal surface. All this information is very valuable in the evaluation of patients with Crohn’s disease.
Also, since SBE and SBFT have represented the standard approach for a long time, they are now commonly used as terms of comparison in evaluating the diagnostic accuracy of all new imaging techniques.
The first attempts to study Crohn’s disease by means of ultrasound (US) date back to the late Seventies[7]. Since then, many studies have addressed the possible role of this technique in diagnosing and monitoring Crohn’s disease with continuous improving quality in US imaging due to evolving technological advancements.
The main ultrasound findings in Crohn’s disease are represented by thickening and stiffness of the gut wall, modifications or lack of its echostratification, reduction of peristalsis, mesenteric fibro-fatty proliferation, lymph node enlargement; in case of complications, narrowing of the intestinal lumen, abscesses and fistula are usually easily detectable (Table 1).
| Features | Crohn’s disease |
| Bowel wall | |
| Thickening | 4-14 mm |
| Echopattern | Variable |
| Vascularity | Variable |
| Contours | Variable |
| Stiffness | Often present |
| Haustra coli | Absent |
| Peristalsis | Often weak or absent |
| Location and extension | |
| Site | Ileum 70% |
| Bowel involvement | Often divided into segments |
| Extra-intestinal alterations | |
| Mesenteric hypertrophy | Common |
| Enlarged regional lymph nodes | Common |
| Fistulae and abscesses | Common |
At least four studies have prospectively compared the diagnostic accuracy of US with that of radiological studies, endoscopy or surgery in suspected Crohn’s disease at diagnosis[8-10]. In these studies, the sensitivity of US ranged between 84% and 90% and its specificity reached 98%-100%.
The capacity of US to detect the exact location of Crohn's disease was also compared with the findings at radiology, endoscopy or surgery in some studies[11-16]. In the largest series[12], the overall sensitivity was 93% and the specificity was 97%, the highest sensitivity (95%) being reached when the disease involved the terminal ileum.
The use of US has also been proposed in the follow-up of patients with known Crohn’s disease, not only when an abdominal complication (i.e. strictures, abscesses or fistula) is suspected, but also in asymptomatic patients in order to identify the occurrence of complication(s) at an earlier stage[17].
Indeed, US compares very well with radiological techniques and surgery, mainly in the detection of strictures and abscesses, while for fistulas data are more conflicting and less satisfactory, with sensitivity values ranging from 50% to 87% and specificity values from 90% to 95%[12,18-22] (Tables 2 and 3).
Repeated US examinations may be of help in the follow-up of Crohn’s disease patients after surgery; indeed, in this setting US is able to detect endoscopic recurrence after resective surgery[23,24]. Also, in one study, in non operated patients, increased bowel thickness was the major risk factor for intestinal resection in the following 12 mo[25]; its persistence after conservative surgery appears to identify those patients at highest risk of clinical and surgical recurrence[26].
The use of US has also been proposed as a possible tool in the assessment of disease activity. However, a weak correlation between US findings and clinical disease severity is usually observed[11,16].
Recently, the use of Power Doppler methods and of oral (polyethylene glycole, PEG) and/or intravenous (Levovist) contrast media, have been suggested to improve the diagnostic accuracy of US, particularly in discriminating inflammatory from fibrotic strictures and in better defining the presence of internal fistulas[27]. These observations are promising, but still too preliminary to suggest the use of these techniques in routine clinical practice.
Since the first studies suggesting its possible role in the management of Crohn’s disease patients[28], Computed Tomography (CT) has usually been utilized for the detection of extra-enteric complications of Crohn's disease, mainly intra-abdominal abscesses, but is also suitable in the evaluation of strictures, prestenotic dilatations and fistulas. Non-enhanced CT scan is also used in the diagnosis of post-surgical complications (intra-peritoneal abscesses, anastomotic deiscence, extra-abdominal abscesses and fistulas, incisional hernias, ascites, volvolus, bowel adhesions, etc.).
This diagnostic technique has also evolved more recently in contrast-enhanced examination, using intravenous administration of iodine contrast agents, and CT-enteroclysis, that can be obtained by means of a fairly large amount (1500 to 2000 mL or more) of contrast agent administered orally or by the positioning of a nasojejunal tube; this technique usually allows the evaluation of the colon as well.
Commonly intravenous and intra-luminal contrast agents are used in combination[29-31]. Various types of intra-luminal contrast media were used to allow negative or positive contrast between the intestinal wall and the lumen[29-35]. Negative intra-luminal contrast agents facilitate the demonstration of normal and diseased bowel segments, particularly after intravenous contrast administration[36].
As a bowel distension media, some authors used a combination of water and iodined contrast agent, or pure water alone. Some authors prefer methylcellulose-water[34]; the latter solution requiring a semi-automatic injector pump.
An appropriate patient preparation with intestinal cleaning should be performed; the small bowel tract should be clean and empty, with lumen distension[32,37,38], avoiding collapsed loops that may mimic wall thickening, strictures and enlarged lymph nodes or abscesses, that can result in diagnostic mistakes[30,33,34].
The intravenous injection of an antiperistaltic drug immediately prior to scanning, blocking the peristalsis, minimizes bowel movement or contraction and allows better intra-luminal distension avoiding the progression of the enteral solution.
A recent study demonstrated that noninvasive peroral CT evaluation of the small bowel is as accurate as CT with jejunal infusion in detecting active small bowel inflammation in Crohn’s disease patients[39].
The main findings at CT scan observed in Crohn’s disease patients, are small bowel wall stratification and/or thickening (“target” or “double halo” appearance), with or without contrast enhancement, oedema of the mesenteric fat, engorged ileal vasa recta (“comb sign”), sub-mucosal fibro-fatty infiltration and mesenteric adenopathy. The pattern and length of mural contrast enhancement should be carefully evaluated. Wall enhancement is a direct expression of trans-mural inflammation; on the contrary, a thickened non-enhancing tract is usually the result of the evolution in submucosal or trans-mural fibrosis. The limited spatial resolution of conventional helical CT images results in lower rates of demonstration of early disease manifestations and of fistulas and sinus tracts, when compared with enteroclysis examinations.
More recently, the development of multislice helical CT scanners improved visualization of the small bowel[40-42], and abdomen in general, both with higher spatial and temporal resolution acquiring isotropic voxel slices in a single breath-hold scan. These examination modalities allow better three dimensional reconstruction methods (multiplanar reconstruction, volume rendering and surface shading display) and volumetric-through navigation (the so called virtual CT-endoscopy).
When compared to endoscopy, small bowel enteroclysis and surgery in the evaluation of small bowel inflammation, CT shows a sensitivity ranging between 71% and 83% and a specificity between 90% and 98%[43,44]. Whether CT scan is also able to assess disease activity in Crohn’s disease patients, remains unclear.
In any case, CT plays a relevant role in the acquisition of additional information on extra-luminal complications (mainly intra-abdominal abscesses) and extra-enteric abnormalities[43].
Also, CT represents the standard technique to guide abscess drainage when ultrasound guided drainage is not possible[44].
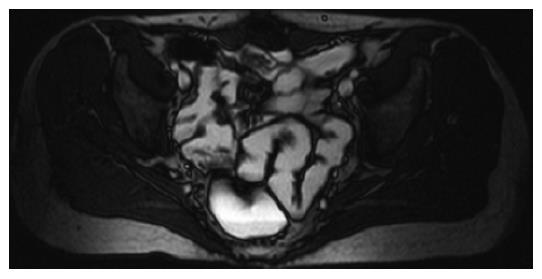
Magnetic resonance (MR) imaging is a non-invasive, non-ionizing radiation diagnostic technique able to obtain multiplanar diagnostic information about intra- and extra-mural involvement of the small bowel by Crohn’s disease and its complications[45-47].
MR evaluation of the small bowel had no clinical application and was still considered an experimental technique until the late Nineties mainly because of poor quality in depicting the gastrointestinal tract. Later, MR technical improvements (multichannel and phased-array coils, faster gradients; fast and ultrafast gradient echo and steady state sequences) allowed a deeper insight into luminal and extra-luminal structures with higher spatial resolution during breath-holding.
Small bowel distension with intra-luminal contrast agent had been known for years in conventional X-ray enteroclysis with barium solution, when it was first reported in publications relating to MR imaging[48-50]. Nowadays, this approach should be considered mandatory in order to obtain bowel loop separation and good contrast resolution between lumen, wall and extra-mural structures.
The first examples of new sequences and bowel distension were reported in the late 1990s[51], comparing spin-echo unenhanced sequences with spoiled gradient-echo images with intra-luminal barium contrast agent and intravenous Gd-base paramagnetic contrast, obtaining greater diagnostic value in identifying small bowel wall abnormalities.
Nowadays, thanks to powerful gradients MR, there is a wide use of fast spin-echo and fast gradient echo sequences that are able to acquire 20-30 slices during a single breath-hold. Spectral fat saturation can be added to T2-weighted sequences to maximize contrast between lumen and wall and between bowels and mesenteric fat[52].
Intra-luminal contrast agents can be administered orally or by nasojejunal catheter (NJC). Contrast media are commonly classified as positive, biphasic or negative, according to their action on signal intensity[53]. Oral administration is obviously better tolerated than the positioning and introduction through an NJC. However, the latter technique allows better distension of the small bowel loops because of higher injection pressure in a shorter time.
The necessity to minimize bowel movements during the acquisition is satisfied using an antiperistaltic drug (usually, joscine N-butylbromure) administered intravenously when the patient is positioned inside the MR unit. The use of intravenous paramagnetic contrast agent is a powerful tool to detect the precise localization of the disease[51], or to evaluate the persistence of inflammation despite active therapy[54,55]. Moreover, it also facilitates the diagnosis of mesenterial abscesses, fistulae, and other abdominal or extra-abdominal complications. Gd-chelates are commonly used, followed by 10-20 mL of saline flush.
Arterial and later acquisition phases can be important to distinguish the submucosal enhancement in the arterial phase, that is a distinctive diagnostic sign of active disease in an intestinal segment, especially if the wall is locally thickened. The optimal contrast enhancement can be achieved using fat-saturated sequences.
Importantly, a good correlation between the degree of wall enhancement after intravenous contrast injection and disease activity, calculated using the Crohn’s Disease Activity Index (CDAI), has been obtained, with an overall high specificity for MR findings[56]. Several recent studies have shown that MR enteroclysis is characterized by high sensitivity and specificity (> 80%) in the diagnosis and evaluation of Crohn’s disease[57-59] (Figures 2 and 3).
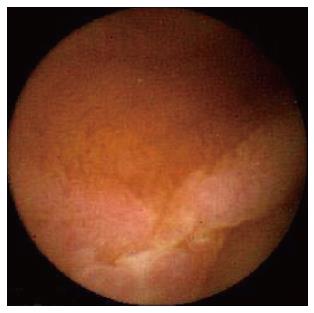
The introduction in clinical practice of VCE has made available, for the first time in history, a potentially safe and painless endoscopic method to evaluate the entire small bowel.
Since its introduction and on the grounds of many papers published in the last five years, VCE has quickly become an essential diagnostic tool in many disease conditions involving the small bowel, although, at the beginning, Crohn’s disease was considered a contraindication for VCE due to the risk of asymptomatic strictures potentially leading to capsule retention.
However, the first suggestion of the possible role of VCE in diagnosing Crohn’s disease came from the unexpected findings of small bowel lesions (observed with a frequency of about 10%) which were suspected for Crohn’s disease (Figures 4 and 5) in several series of patients who had been evaluated for obscure gastrointestinal bleeding[60-63]. Most of these patients only had obscure gastrointestinal bleeding with no symptoms of Crohn’s disease and had been thoroughly evaluated with an extensive endoscopic and radiologic diagnostic work-up before performing VCE. Thus, the presence of these unexpected findings at VCE suggested its superiority in detecting Crohn’s disease lesions in patients with mild clinical suspicion and negative traditional imaging studies. Indeed, in this clinical setting, VCE appears to be superior to the other, most frequently used, diagnostic techniques (SBE, SBFT, retrograde ileoscopy, entero-CT and entero-MR) although a recent meta-analysis failed to show statistically significant differences in the diagnostic yields of VCE versus other imaging techniques[63-71] (Table 4).
| Yield ofcapsuleendoscopy (%) | Yield of othermodalities(%) | % Incrementalyield for capsuleendoscopy (95% CI) | P | |
| vs Small bowel radiography | 43 | 13 | 24 (-0.3-0.51) | 0.09 |
| vs Ileoscopy | 33 | 26 | 7 (-0.12-0.25) | 0.48 |
| vs CT enterography | 70 | 21 | 40 (-0.03-0.83) | 0.07 |
A recent, single-centre, prospective study[72] evaluated the accuracy of VCE in diagnosing Crohn’s disease in a cohort of patients with suspicion of the disease (defined as diarrhoea of more than three months duration accompanied by anaemia, and/or weight loss, and/or fever, and/or extra-intestinal manifestations) after 21 mo of follow-up. This study showed high sensitivity, specificity and positive and negative likelihood ratio (93%, 84%, 5.8 and 0.08, respectively) of this new diagnostic tool in diagnosing Crohn’s disease.
The role of VCE has also been assessed in patients with known Crohn’s disease. Several recent studies[63,73-78] highlighted the superior diagnostic yield of VCE (ranging from 61% to 77%) when compared to that of SBFT, SBE or entero-CT (ranging from 19% to 26%) in assessing small bowel involvement in patients with a previous diagnosis of Crohn’s disease. In this setting, VCE appears to have a superior capability in evaluating the extent of small bowel involvement when compared with push enteroscopy[76,78] (Table 5).
| Yield ofcapsuleendoscopy(%) | Yield ofothermodalities(%) | % Incrementalyield for capsuleendoscopy(95% CI) | NNT | P | |
| vs Small bowel radiography | 78 | 32 | 51 (0.31-0.70) | 2 | < 0.001 |
| vs Ileoscopy | 86 | 60 | 26 (0.08-0.43) | 4 | 0.002 |
| vs CT enterography | 68 | 38 | 30 (0.12-0.48) | - | < 0.01 |
There are, however, some limitations to take into account in evaluating these data. In patients with clinically suspected Crohn’s disease with no further evidence of the disease, one should be cautious in interpreting VCE findings. In fact, the significance of isolated lesions or mucosal breaks in the small bowel is not clear, since they may be observed also in normal subjects[79], and more frequently in subjects taking NSAIDs[66,79]. Thus, before giving a diagnosis of Crohn’s disease to a patient with VCE small bowel lesions only, a careful and thorough clinical evaluation should be performed.
Performing VCE may be helpful in evaluating patients with indeterminate colitis (IC). Indeed, in some series[80,81], 20%-50% of IC patients are characterized by the presence of small bowel lesions, leading to a change in their diagnostic definition.
Further possible applications of VCE have been suggested in a paediatric setting[82], in the evaluation of post-surgical recurrence[64] and in the surveillance of mucosal healing after biologic therapy[64].
The major limitations of the use of VCE in Crohn’s disease are represented by an incomplete evaluation of the small bowel, occurring in 20%-35% of patients[83,84], and by the possibility of capsule retention, occurring in 1%, 4%-6%, 7% of patients with Crohn’s disease[85]. To avoid this complication, it is debated whether or not radiological study should be performed before VCE[85]. Further studies are also needed to clarify the possible role of a time-controlled dissolving capsule to be performed before VCE[86-88].
Double balloon enteroscopy (also called push and pull enteroscopy) was described for the first time by Yamamoto et al[89] in 2001.
The principle of the double balloon technique allows not only a complete endoscopic evaluation of the small bowel but also makes it possible to take biopsies and to carry out therapeutic interventions along the whole small bowel[90,91]. However, even though double balloon enteroscopy appears a safe and useful technique, when compared with VCE it results in an inconvenient and invasive procedure requiring specialized equipment, sedation of patients, fluoroscopy and prolonged examination time.
Preliminary data suggest its possible use in the diagnosis of Crohn’s disease[90,91]; however, to date, there are no published studies comparing double balloon enteroscopy with capsule endoscopy or other imaging modalities in the diagnosis of small bowel Crohn’s disease.
In recent years, several radiologic and endoscopic techni-ques have been developed for the study of the small bowel. Each of these techniques is characterized by its own profile of favourable and unfavourable features. The main pros and cons of the different techniques used for the evaluation of the small bowel in Crohn’s disease are summarized in Table 6.
| PROs | CONs | |
| Bowel ultrasound | -Non invasive, safe and well accepted -Widely available -Information about gut wall and extra-intestinal structures | -Operator dependent -False negative in case of superficial and rare lesions |
| Conventional radiology | -Exact anatomic location and extent of the lesions | -Limited information about trans-mural and peri-intestinal abnormalities -Radiation exposure |
| Entero MR | -Information about gut and extra-intestinal structures -Identification of active inflammation -Multiplanar sequences | -costly -Impossible to enter the magnet -IV infusion |
| Entero CT | -Information about gut and extra-intestinal structures -Mulitplanar sequences | -Radiation exposure -IV infusion -False negative in case of superficial and rare lesions |
| VCE | -Allows the complete evaluation of the small bowel -High diagnostic yield -Useful in indeterminate colitis -Well tolerated | -Unfeasible if significant stricture present -Not well established specificity of VCE findings |
| Double-balloon | -Allows the complete evaluation of the small bowel -Therapy and biopsies are feasible | -Invasive procedure requiring sedation and fluoroscopy -No data |
Ultrasound and entero-MR appear to be particularly interesting, since neither of them use ionizing radiation. The main advantage of MR 'enteroclisys' over ultrasound is the panoramic view over the whole abdominal cavity, allowing the detection of disease involvement in other gastrointestinal segments or abdominal organs. Moreover, ultrasound is an operator-dependent technique and its use is limited in patients with a large abdomen[12]. On the other hand, ultrasound is a low cost and easily available diagnostic tool.
Thus, we believe that when the diagnosis of Crohn’s disease is established and we want to investigate the small bowel, one of these two tests should be performed, and the choice should be based on the presence and availability of the techniques and of experienced operators in the area.
A different choice may be performed when the diagnosis has to be reached, particularly in patients suspected of Crohn’s disease and negative upper and lower endoscopy. In these cases, endoscopy appears to be superior to all other techniques, particularly when minute lesions are suspected; thus, capsule endoscopy (when no suspicion of a significant stricture exists) or double balloon enteroscopy should be the preferred tests to be performed. In cases of only isolated lesions and in the absence of a typical histological picture, one should be cautious before making a diagnosis of Crohn’s disease on the basis of these findings only.
In general, when we care for patients with Crohn's disease we should always keep in mind that, during the natural course of the disease, these patients will undergo repeated examinations in their follow-up: thus, our goals should always be (1) to perform tests only when they are expected to provide important clues for the management of the patients and (2) to choose those tests with the best profile of diagnostic accuracy and safety.
Keeping this in mind, we have to recognize that all these new developments have opened a new and exciting area in the exploration of the small bowel.
We are indebted to Dr. Antonella Bianchi for her very valuable technical help.
Crohn’s disease often affects the small bowel and is characterised by the occurrence of several intra- and extra-luminal complications. The study of the small bowel is mandatory in patients with Crohn’s disease. In the last years, several techniques have been proposed for the imaging of the small bowel as possible alternatives to the traditional ones.
To point out the most recent advances in the study of the small bowel in patients with suspected or proven Crohn’s disease.
To critically evaluate the advantages and the disadvantages of ultrasonography, radiology and endoscopy in the diagnosis and the surveillance of Crohn’s disease affecting the small bowel.
To optimize the use of the several imaging techniques now available when one care for patients affected by Crohn’s disease with small bowel localization.
To concisely and accurately describe, define or explain the specific, unique terms that are not familiar to the majority of the readers, but are essential for the readers to understand the article.
Valuable review of investigational techniques for Crohn’s disease.
S- Editor Liu Y L- Editor Roberts SE E- Editor Lu W
| 1. | Ranzi T, Bodini P, Zambelli A, Politi P, Lupinacci G, Campanini MC, Dal Lago AL, Lisciandrano D, Bianchi PA. Epidemiological aspects of inflammatory bowel disease in a north Italian population: a 4-year prospective study. Eur J Gastroenterol Hepatol. 1996;8:657-661. [PubMed] |
| 2. | Fraser GM, Findlay JM. The double contrast enema in ulcerative and Crohn's colitis. Clin Radiol. 1976;27:103-112. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 42] [Cited by in RCA: 41] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 3. | Laufer I, Hamilton J. The radiological differentiation between ulcerative and granulomatous colitis by double contrast radiology. Am J Gastroenterol. 1976;66:259-269. [PubMed] |
| 4. | Kelvin FM, Maglinte DD. Enteroclysis or small bowel follow-through in Crohn' s diseases? Gastroenterology. 1998;114:1349-1351. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 17] [Cited by in RCA: 20] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 5. | Bernstein CN, Boult IF, Greenberg HM, van der Putten W, Duffy G, Grahame GR. A prospective randomized comparison between small bowel enteroclysis and small bowel follow-through in Crohn's disease. Gastroenterology. 1997;113:390-398. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 83] [Cited by in RCA: 87] [Article Influence: 3.1] [Reference Citation Analysis (0)] |
| 6. | Gasche C, Schober E, Turetschek K. Small bowel barium studies in Crohn's disease. Gastroenterology. 1998;114:1349. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 9] [Cited by in RCA: 10] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 7. | Holt S, Samuel E. Grey scale ultrasound in Crohn's disease. Gut. 1979;20:590-595. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 53] [Cited by in RCA: 56] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 8. | Bozkurt T, Richter F, Lux G. Ultrasonography as a primary diagnostic tool in patients with inflammatory disease and tumors of the small intestine and large bowel. J Clin Ultrasound. 1994;22:85-91. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 62] [Cited by in RCA: 49] [Article Influence: 1.6] [Reference Citation Analysis (0)] |
| 9. | Hollerbach S, Geissler A, Schiegl H, Kullmann F, Lock G, Schmidt J, Schlegel J, Schoelmerich J, Andus T. The accuracy of abdominal ultrasound in the assessment of bowel disorders. Scand J Gastroenterol. 1998;33:1201-1208. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 80] [Cited by in RCA: 82] [Article Influence: 3.0] [Reference Citation Analysis (0)] |
| 10. | Astegiano M, Bresso F, Cammarota T, Sarno A, Robotti D, Demarchi B, Sostegni R, Macchiarella V, Pera A, Rizzetto M. Abdominal pain and bowel dysfunction: diagnostic role of intestinal ultrasound. Eur J Gastroenterol Hepatol. 2001;13:927-931. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 42] [Cited by in RCA: 34] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 11. | Maconi G, Parente F, Bollani S, Cesana B, Bianchi Porro G. Abdominal ultrasound in the assessment of extent and activity of Crohn's disease: clinical significance and implication of bowel wall thickening. Am J Gastroenterol. 1996;91:1604-1609. [PubMed] |
| 12. | Parente F, Maconi G, Bollani S, Anderloni A, Sampietro G, Cristaldi M, Franceschelli N, Bianco R, Taschieri AM, Bianchi Porro G. Bowel ultrasound in assessment of Crohn's disease and detection of related small bowel strictures: a prospective comparative study versus x ray and intraoperative findings. Gut. 2002;50:490-495. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 136] [Cited by in RCA: 121] [Article Influence: 5.3] [Reference Citation Analysis (0)] |
| 13. | Brignola C, Belloli C, Iannone P, De Simone G, Corbelli C, Levorato M, Arienti V, Boriani L, Gionchetti P, Belluzzi A. Comparison of scintigraphy with indium-111 leukocyte scan and ultrasonography in assessment of X-ray-demonstrated lesions of Crohn's disease. Dig Dis Sci. 1993;38:433-437. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 25] [Cited by in RCA: 25] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 14. | Solvig J, Ekberg O, Lindgren S, Florén CH, Nilsson P. Ultrasound examination of the small bowel: comparison with enteroclysis in patients with Crohn disease. Abdom Imaging. 1995;20:323-326. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 47] [Cited by in RCA: 49] [Article Influence: 1.6] [Reference Citation Analysis (0)] |
| 15. | Haber HP, Busch A, Ziebach R, Dette S, Ruck P, Stern M. Ultrasonographic findings correspond to clinical, endoscopic, and histologic findings in inflammatory bowel disease and other enterocolitides. J Ultrasound Med. 2002;21:375-382. [PubMed] |
| 16. | Parente F, Greco S, Molteni M, Cucino C, Maconi G, Sampietro GM, Danelli PG, Cristaldi M, Bianco R, Gallus S. Role of early ultrasound in detecting inflammatory intestinal disorders and identifying their anatomical location within the bowel. Aliment Pharmacol Ther. 2003;18:1009-1016. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 146] [Cited by in RCA: 142] [Article Influence: 6.5] [Reference Citation Analysis (0)] |
| 17. | Hirche TO, Russler J, Schröder O, Schuessler G, Kappeser P, Caspary WF, Dietrich CF. The value of routinely performed ultrasonography in patients with Crohn disease. Scand J Gastroenterol. 2002;37:1178-1183. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 48] [Cited by in RCA: 42] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 18. | Maconi G, Bollani S, Bianchi Porro G. Ultrasonographic detection of intestinal complications in Crohn's disease. Dig Dis Sci. 1996;41:1643-1648. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 103] [Cited by in RCA: 92] [Article Influence: 3.2] [Reference Citation Analysis (0)] |
| 19. | Gasche C, Moser G, Turetschek K, Schober E, Moeschl P, Oberhuber G. Transabdominal bowel sonography for the detection of intestinal complications in Crohn's disease. Gut. 1999;44:112-117. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 149] [Cited by in RCA: 142] [Article Influence: 5.5] [Reference Citation Analysis (0)] |
| 20. | Kohn A, Cerro P, Milite G, De Angelis E, Prantera C. Prospective evaluation of transabdominal bowel sonography in the diagnosis of intestinal obstruction in Crohn's disease: comparison with plain abdominal film and small bowel enteroclysis. Inflamm Bowel Dis. 1999;5:153-157. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 35] [Cited by in RCA: 42] [Article Influence: 1.6] [Reference Citation Analysis (0)] |
| 21. | Maconi G, Sampietro GM, Parente F, Pompili G, Russo A, Cristaldi M, Arborio G, Ardizzone S, Matacena G, Taschieri AM. Contrast radiology, computed tomography and ultrasonography in detecting internal fistulas and intra-abdominal abscesses in Crohn's disease: a prospective comparative study. Am J Gastroenterol. 2003;98:1545-1555. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 156] [Cited by in RCA: 140] [Article Influence: 6.4] [Reference Citation Analysis (0)] |
| 22. | Parente F, Greco S, Molteni M, Anderloni A, Maconi G, Bianchi Porro G. Modern imaging of Crohn's disease using bowel ultrasound. Inflamm Bowel Dis. 2004;10:452-461. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 53] [Cited by in RCA: 45] [Article Influence: 2.1] [Reference Citation Analysis (0)] |
| 23. | DiCandio G, Mosca F, Campatelli A, Bianchini M, D'Elia F, Dellagiovampaola C. Sonographic detection of postsurgical recurrence of Crohn disease. AJR Am J Roentgenol. 1986;146:523-526. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 47] [Cited by in RCA: 51] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 24. | Andreoli A, Cerro P, Falasco G, Giglio LA, Prantera C. Role of ultrasonography in the diagnosis of postsurgical recurrence of Crohn's disease. Am J Gastroenterol. 1998;93:1117-1121. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 58] [Cited by in RCA: 59] [Article Influence: 2.2] [Reference Citation Analysis (0)] |
| 25. | Castiglione F, de Sio I, Cozzolino A, Rispo A, Manguso F, Del Vecchio Blanco G, Di Girolamo E, Castellano L, Ciacci C, Mazzacca G. Bowel wall thickness at abdominal ultrasound and the one-year-risk of surgery in patients with Crohn's disease. Am J Gastroenterol. 2004;99:1977-1983. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 55] [Cited by in RCA: 50] [Article Influence: 2.4] [Reference Citation Analysis (0)] |
| 26. | Maconi G, Sampietro GM, Cristaldi M, Danelli PG, Russo A, Bianchi Porro G, Taschieri AM. Preoperative characteristics and postoperative behavior of bowel wall on risk of recurrence after conservative surgery in Crohn's disease: a prospective study. Ann Surg. 2001;233:345-352. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 62] [Cited by in RCA: 63] [Article Influence: 2.6] [Reference Citation Analysis (0)] |
| 27. | Parente F, Greco S, Molteni M, Anderloni A, Bianchi Porro G. Imaging inflammatory bowel disease using bowel ultrasound. Eur J Gastroenterol Hepatol. 2005;17:283-291. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 52] [Cited by in RCA: 40] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 28. | Berliner L, Redmond P, Purow E, Megna D, Sottile V. Computed tomography in Crohn's disease. Am J Gastroenterol. 1982;77:548-553. [PubMed] |
| 29. | Makó EK, Mester AR, Tarján Z, Karlinger K, Tóth G. Enteroclysis and spiral CT examination in diagnosis and evaluation of small bowel Crohn's disease. Eur J Radiol. 2000;35:168-175. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 70] [Cited by in RCA: 71] [Article Influence: 2.8] [Reference Citation Analysis (0)] |
| 30. | Rollandi GA, Curone PF, Biscaldi E, Nardi F, Bonifacino E, Conzi R, Derchi LE. Spiral CT of the abdomen after distention of small bowel loops with transparent enema in patients with Crohn's disease. Abdom Imaging. 1999;24:544-549. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 83] [Cited by in RCA: 84] [Article Influence: 3.2] [Reference Citation Analysis (0)] |
| 31. | Turetschek K, Schober E, Wunderbaldinger P, Bernhard C, Schima W, Puespoek A, Vogelsang H, Moeschl P, Mostbeck G. Findings at helical CT-enteroclysis in symptomatic patients with crohn disease: correlation with endoscopic and surgical findings. J Comput Assist Tomogr. 2002;26:488-492. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 59] [Cited by in RCA: 48] [Article Influence: 2.1] [Reference Citation Analysis (0)] |
| 32. | Furukawa A, Yamasaki M, Furuichi K, Yokoyama K, Nagata T, Takahashi M, Murata K, Sakamoto T. Helical CT in the diagnosis of small bowel obstruction. Radiographics. 2001;21:341-355. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 142] [Cited by in RCA: 102] [Article Influence: 4.3] [Reference Citation Analysis (0)] |
| 33. | Gore RM, Balthazar EJ, Ghahremani GG, Miller FH. CT features of ulcerative colitis and Crohn's disease. AJR Am J Roentgenol. 1996;167:3-15. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 281] [Cited by in RCA: 290] [Article Influence: 10.0] [Reference Citation Analysis (0)] |
| 34. | Herliger H, Maglinte DDT. The small bowel enema with methylcellulose. Clinical radiology of the small intestine. Philadelphia, Pa: Saunders 1989; 119-137. |
| 35. | Raptopoulos V, Schwartz RK, McNicholas MM, Movson J, Pearlman J, Joffe N. Multiplanar helical CT enterography in patients with Crohn's disease. AJR Am J Roentgenol. 1997;169:1545-1550. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 127] [Cited by in RCA: 105] [Article Influence: 3.8] [Reference Citation Analysis (0)] |
| 36. | Furukawa A, Saotome T, Yamasaki M, Maeda K, Nitta N, Takahashi M, Tsujikawa T, Fujiyama Y, Murata K, Sakamoto T. Cross-sectional imaging in Crohn disease. Radiographics. 2004;24:689-702. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 194] [Cited by in RCA: 135] [Article Influence: 6.4] [Reference Citation Analysis (0)] |
| 37. | Desai RK, Tagliabue JR, Wegryn SA, Einstein DM. CT evaluation of wall thickening in the alimentary tract. Radiographics. 1991;11:771-783; discussion 784. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 86] [Cited by in RCA: 72] [Article Influence: 2.1] [Reference Citation Analysis (0)] |
| 38. | Balthazar EJ. CT of the gastrointestinal tract: principles and interpretation. AJR Am J Roentgenol. 1991;156:23-32. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 170] [Cited by in RCA: 173] [Article Influence: 5.1] [Reference Citation Analysis (0)] |
| 39. | Wold PB, Fletcher JG, Johnson CD, Sandborn WJ. Assessment of small bowel Crohn disease: noninvasive peroral CT enterography compared with other imaging methods and endoscopy--feasibility study. Radiology. 2003;229:275-281. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 255] [Cited by in RCA: 263] [Article Influence: 12.0] [Reference Citation Analysis (0)] |
| 40. | Maglinte DD, Bender GN, Heitkamp DE, Lappas JC, Kelvin FM. Multidetector-row helical CT enteroclysis. Radiol Clin North Am. 2003;41:249-262. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 103] [Cited by in RCA: 107] [Article Influence: 4.9] [Reference Citation Analysis (0)] |
| 41. | Molnár T, Papós M, Gyulai C, Ambrus E, Kardos L, Nagy F, Palkó A, Pávics L, Lonovics J. Clinical value of technetium-99m-HMPAO-labeled leukocyte scintigraphy and spiral computed tomography in active Crohn's disease. Am J Gastroenterol. 2001;96:1517-1521. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 27] [Cited by in RCA: 26] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 42. | Kolkman JJ, Falke TH, Roos JC, Van Dijk DH, Bannink IM, Den Hollander W, Cuesta MA, Peña AS, Meuwissen SG. Computed tomography and granulocyte scintigraphy in active inflammatory bowel disease. Comparison with endoscopy and operative findings. Dig Dis Sci. 1996;41:641-650. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 46] [Cited by in RCA: 45] [Article Influence: 1.6] [Reference Citation Analysis (0)] |
| 43. | Schreyer AG, Seitz J, Feuerbach S, Rogler G, Herfarth H. Modern imaging using computer tomography and magnetic resonance imaging for inflammatory bowel disease (IBD) AU1. Inflamm Bowel Dis. 2004;10:45-54. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 65] [Cited by in RCA: 59] [Article Influence: 2.8] [Reference Citation Analysis (0)] |
| 44. | Casola G, vanSonnenberg E, Neff CC, Saba RM, Withers C, Emarine CW. Abscesses in Crohn disease: percutaneous drainage. Radiology. 1987;163:19-22. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 101] [Cited by in RCA: 101] [Article Influence: 2.7] [Reference Citation Analysis (0)] |
| 45. | Umschaden HW, Szolar D, Gasser J, Umschaden M, Haselbach H. Small-bowel disease: comparison of MR enteroclysis images with conventional enteroclysis and surgical findings. Radiology. 2000;215:717-725. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 213] [Cited by in RCA: 220] [Article Influence: 8.8] [Reference Citation Analysis (0)] |
| 46. | Prassopoulos P, Papanikolaou N, Grammatikakis J, Rousomoustakaki M, Maris T, Gourtsoyiannis N. MR enteroclysis imaging of Crohn disease. Radiographics. 2001;21 Spec No:S161-S172. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 163] [Cited by in RCA: 166] [Article Influence: 6.9] [Reference Citation Analysis (0)] |
| 47. | Laghi A, Passariello R. Magnetic Resonance in the study of the small bowel. Radiol Med. 2003;106:1-15; quiz 16-17. [PubMed] |
| 48. | Wesbey GE, Brasch RC, Goldberg HI, Engelstad BL, Moss AA. Dilute oral iron solutions as gastrointestinal contrast agents for magnetic resonance imaging; initial clinical experience. Magn Reson Imaging. 1985;3:57-64. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 48] [Cited by in RCA: 49] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 49. | Tart RP, Li KC, Storm BL, Rolfes RJ, Ang PG. Enteric MRI contrast agents: comparative study of five potential agents in humans. Magn Reson Imaging. 1991;9:559-568. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 17] [Cited by in RCA: 18] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 50. | Sardanelli F, de Cicco E, Renzetti P, Parodi RC, Calabrese M. Double-contrast magnetic resonance examination of ulcerative colitis. Eur Radiol. 1999;9:875-879. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 9] [Cited by in RCA: 10] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 51. | Low RN, Francis IR. MR imaging of the gastrointestinal tract with i.v., gadolinium and diluted barium oral contrast media compared with unenhanced MR imaging and CT. AJR Am J Roentgenol. 1997;169:1051-1059. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 83] [Cited by in RCA: 86] [Article Influence: 3.1] [Reference Citation Analysis (0)] |
| 52. | Gourtsoyiannis N, Papanikolaou N, Grammatikakis J, Maris T, Prassopoulos P. MR imaging of the small bowel with a true-FISP sequence after enteroclysis with water solution. Invest Radiol. 2000;35:707-711. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 71] [Cited by in RCA: 73] [Article Influence: 2.9] [Reference Citation Analysis (0)] |
| 53. | Debatin JF, Patak MA. MRI of the small and large bowel. Eur Radiol. 1999;9:1523-1534. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 52] [Cited by in RCA: 55] [Article Influence: 2.1] [Reference Citation Analysis (0)] |
| 54. | Madsen SM, Thomsen HS, Schlichting P, Dorph S, Munkholm P. Evaluation of treatment response in active Crohn's disease by low-field magnetic resonance imaging. Abdom Imaging. 1999;24:232-239. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 47] [Cited by in RCA: 49] [Article Influence: 1.9] [Reference Citation Analysis (0)] |
| 55. | Durno CA, Sherman P, Williams T, Shuckett B, Dupuis A, Griffiths AM. Magnetic resonance imaging to distinguish the type and severity of pediatric inflammatory bowel diseases. J Pediatr Gastroenterol Nutr. 2000;30:170-174. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 52] [Cited by in RCA: 55] [Article Influence: 2.2] [Reference Citation Analysis (0)] |
| 56. | Koh DM, Miao Y, Chinn RJ, Amin Z, Zeegen R, Westaby D, Healy JC. MR imaging evaluation of the activity of Crohn's disease. AJR Am J Roentgenol. 2001;177:1325-1332. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 288] [Cited by in RCA: 299] [Article Influence: 12.5] [Reference Citation Analysis (0)] |
| 57. | Röttgen R, Herzog H, Lopez-Hänninen E, Cho CH, Felix R, Schröder RJ. [Combination of dynamic MR enteroclysis (Sellink) and MR colonography to diagnose Crohn's disease]. Rofo. 2005;177:1131-1138. [PubMed] |
| 58. | Masselli G, Brizi MG, Menchini L, Minordi L, Vecchioli Scaldazza A. Magnetic Resonance Enteroclysis imaging of Crohn's. Radiol Med. 2005;110:221-233. [PubMed] |
| 59. | Godefroy C, Pilleul F, Dugougeat F, Yzèbe D, Lachaux A, Pracros JP, Valette PJ. [Value of contrast-enhanced MR enterography in pediatric Crohn's disease: preliminary study]. J Radiol. 2005;86:1685-1692. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 24] [Cited by in RCA: 26] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 60. | Ell C, Remke S, May A, Helou L, Henrich R, Mayer G. The first prospective controlled trial comparing wireless capsule endoscopy with push enteroscopy in chronic gastrointestinal bleeding. Endoscopy. 2002;34:685-689. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 435] [Cited by in RCA: 407] [Article Influence: 17.7] [Reference Citation Analysis (0)] |
| 61. | Costamagna G, Shah SK, Riccioni ME, Foschia F, Mutignani M, Perri V, Vecchioli A, Brizi MG, Picciocchi A, Marano P. A prospective trial comparing small bowel radiographs and video capsule endoscopy for suspected small bowel disease. Gastroenterology. 2002;123:999-1005. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 565] [Cited by in RCA: 517] [Article Influence: 22.5] [Reference Citation Analysis (0)] |
| 62. | Lo SK. Capsule endoscopy in the diagnosis and management of inflammatory bowel disease. Gastrointest Endosc Clin N Am. 2004;14:179-193. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 24] [Cited by in RCA: 28] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 63. | Triester SL, Leighton JA, Leontiadis GI, Gurudu SR, Fleischer DE, Hara AK, Heigh RI, Shiff AD, Sharma VK. A meta-analysis of the yield of capsule endoscopy compared to other diagnostic modalities in patients with non-stricturing small bowel Crohn's disease. Am J Gastroenterol. 2006;101:954-964. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 392] [Cited by in RCA: 355] [Article Influence: 18.7] [Reference Citation Analysis (1)] |
| 64. | Kornbluth A, Legnani P, Lewis BS. Video capsule endoscopy in inflammatory bowel disease: past, present, and future. Inflamm Bowel Dis. 2004;10:278-285. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 58] [Cited by in RCA: 52] [Article Influence: 2.5] [Reference Citation Analysis (0)] |
| 65. | Fireman Z, Mahajna E, Broide E, Shapiro M, Fich L, Sternberg A, Kopelman Y, Scapa E. Diagnosing small bowel Crohn's disease with wireless capsule endoscopy. Gut. 2003;52:390-392. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 281] [Cited by in RCA: 270] [Article Influence: 12.3] [Reference Citation Analysis (0)] |
| 66. | Herrerías JM, Caunedo A, Rodríguez-Téllez M, Pellicer F, Herrerías JM. Capsule endoscopy in patients with suspected Crohn's disease and negative endoscopy. Endoscopy. 2003;35:564-568. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 146] [Cited by in RCA: 167] [Article Influence: 7.6] [Reference Citation Analysis (0)] |
| 67. | Eliakim R, Adler SN. Capsule video endoscopy in Crohn's disease-the European experience. Gastrointest Endosc Clin N Am. 2004;14:129-137. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 20] [Cited by in RCA: 19] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 68. | Mascarenhas-Saraiva M, Lopes L, Mascarenhas-Saraiva A. A wireless capsule endoscopy is applicable in diagnosing and monitoring of small bowel Croh's disease. Gut. 2002;51S:A69. |
| 69. | Papadakis KA, Lo SK, Fireman Z, Hollerbach S. Wireless capsule endoscopy in the evaluation of patients with suspected or known Crohn's disease. Endoscopy. 2005;37:1018-1022. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 29] [Cited by in RCA: 33] [Article Influence: 1.7] [Reference Citation Analysis (0)] |
| 70. | Mow WS, Lo SK, Targan SR, Dubinsky MC, Treyzon L, Abreu-Martin MT, Papadakis KA, Vasiliauskas EA. Initial experience with wireless capsule enteroscopy in the diagnosis and management of inflammatory bowel disease. Clin Gastroenterol Hepatol. 2004;2:31-40. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 216] [Cited by in RCA: 188] [Article Influence: 9.0] [Reference Citation Analysis (0)] |
| 71. | Eliakim R, Suissa A, Yassin K, Katz D, Fischer D. Wireless capsule video endoscopy compared to barium follow-through and computerised tomography in patients with suspected Crohn's disease--final report. Dig Liver Dis. 2004;36:519-522. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 124] [Cited by in RCA: 121] [Article Influence: 5.8] [Reference Citation Analysis (0)] |
| 72. | Girelli CM, Porta P, Malacrida V, Barzaghi F, Rocca F. Clinical outcome of patients examined by capsule endoscopy for suspected small bowel Crohn's disease. Dig Liver Dis. 2007;39:148-154. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 44] [Cited by in RCA: 49] [Article Influence: 2.7] [Reference Citation Analysis (0)] |
| 73. | Hara AK, Leighton JA, Heigh RI, Sharma VK, Silva AC, De Petris G, Hentz JG, Fleischer DE. Crohn disease of the small bowel: preliminary comparison among CT enterography, capsule endoscopy, small-bowel follow-through, and ileoscopy. Radiology. 2006;238:128-134. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 226] [Cited by in RCA: 239] [Article Influence: 12.6] [Reference Citation Analysis (0)] |
| 74. | Albert JG, Martiny F, Krummenerl A, Stock K, Lesske J, Göbel CM, Lotterer E, Nietsch HH, Behrmann C, Fleig WE. Diagnosis of small bowel Crohn's disease: a prospective comparison of capsule endoscopy with magnetic resonance imaging and fluoroscopic enteroclysis. Gut. 2005;54:1721-1727. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 225] [Cited by in RCA: 188] [Article Influence: 9.4] [Reference Citation Analysis (0)] |
| 75. | Voderholzer WA, Beinhoelzl J, Rogalla P, Murrer S, Schachschal G, Lochs H, Ortner MA. Small bowel involvement in Crohn's disease: a prospective comparison of wireless capsule endoscopy and computed tomography enteroclysis. Gut. 2005;54:369-373. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 239] [Cited by in RCA: 233] [Article Influence: 11.7] [Reference Citation Analysis (0)] |
| 76. | Chong AK, Taylor A, Miller A, Hennessy O, Connell W, Desmond P. Capsule endoscopy vs. push enteroscopy and enteroclysis in suspected small-bowel Crohn's disease. Gastrointest Endosc. 2005;61:255-261. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 113] [Cited by in RCA: 121] [Article Influence: 6.1] [Reference Citation Analysis (0)] |
| 77. | Marmo R, Rotondano G, Piscopo R, Bianco MA, Siani A, Catalano O, Cipolletta L. Capsule endoscopy versus enteroclysis in the detection of small-bowel involvement in Crohn's disease: a prospective trial. Clin Gastroenterol Hepatol. 2005;3:772-776. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 91] [Cited by in RCA: 96] [Article Influence: 4.8] [Reference Citation Analysis (0)] |
| 78. | Mylonaki M, Fritscher-Ravens A, Swain P. Wireless capsule endoscopy: a comparison with push enteroscopy in patients with gastroscopy and colonoscopy negative gastrointestinal bleeding. Gut. 2003;52:1122-1126. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 342] [Cited by in RCA: 372] [Article Influence: 16.9] [Reference Citation Analysis (0)] |
| 79. | Delvaux M. Capsule endoscopy in 2005: facts and perspectives. Best Pract Res Clin Gastroenterol. 2006;20:23-39. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 41] [Cited by in RCA: 52] [Article Influence: 2.7] [Reference Citation Analysis (0)] |
| 80. | Leighton JA, Legnani P, Seidman EG. Role of capsule endoscopy in inflammatory bowel disease: where we are and where we are going. Inflamm Bowel Dis. 2007;13:331-337. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 35] [Cited by in RCA: 35] [Article Influence: 1.9] [Reference Citation Analysis (0)] |
| 81. | Maunoury V, Savoye G, Bourreille A, Bouhnik Y, Jarry M, Sacher-Huvelin S, Ben Soussan E, Lerebours E, Galmiche JP, Colombel JF. Value of wireless capsule endoscopy in patients with indeterminate colitis (inflammatory bowel disease type unclassified). Inflamm Bowel Dis. 2007;13:152-155. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 94] [Cited by in RCA: 80] [Article Influence: 4.4] [Reference Citation Analysis (0)] |
| 82. | Ge ZZ, Chen HY, Gao YJ, Gu JL, Hu YB, Xiao SD. Clinical application of wireless capsule endoscopy in pediatric patients for suspected small bowel diseases. Eur J Pediatr. 2007;166:825-829. [PubMed] |
| 83. | Rondonotti E, Herrerias JM, Pennazio M, Caunedo A, Mascarenhas-Saraiva M, de Franchis R. Complications, limitations, and failures of capsule endoscopy: a review of 733 cases. Gastrointest Endosc. 2005;62:712-716; quiz 752, 754. [PubMed] |
| 84. | Melmed GY, Lo SK. Capsule endoscopy: practical applications. Clin Gastroenterol Hepatol. 2005;3:411-422. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 36] [Cited by in RCA: 45] [Article Influence: 2.3] [Reference Citation Analysis (0)] |
| 85. | Lewis B. How to prevent endoscopic capsule retention. Endoscopy. 2005;37:852-856. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 22] [Cited by in RCA: 25] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 86. | Kornbluth A, Colombel JF, Leighton JA, Loftus E. ICCE consensus for inflammatory bowel disease. Endoscopy. 2005;37:1051-1054. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 89] [Cited by in RCA: 71] [Article Influence: 3.6] [Reference Citation Analysis (0)] |
| 87. | Spada C, Spera G, Riccioni M, Biancone L, Petruzziello L, Tringali A, Familiari P, Marchese M, Onder G, Mutignani M. A novel diagnostic tool for detecting functional patency of the small bowel: the Given patency capsule. Endoscopy. 2005;37:793-800. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 111] [Cited by in RCA: 82] [Article Influence: 4.1] [Reference Citation Analysis (0)] |
| 88. | Boivin ML, Lochs H, Voderholzer WA. Does passage of a patency capsule indicate small-bowel patency? A prospective clinical trial? Endoscopy. 2005;37:808-815. [PubMed] |
| 89. | Yamamoto H, Sekine Y, Sato Y, Higashizawa T, Miyata T, Iino S, Ido K, Sugano K. Total enteroscopy with a nonsurgical steerable double-balloon method. Gastrointest Endosc. 2001;53:216-220. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 896] [Cited by in RCA: 856] [Article Influence: 35.7] [Reference Citation Analysis (0)] |
| 90. | Yamamoto H, Kita H, Sunada K, Hayashi Y, Sato H, Yano T, Iwamoto M, Sekine Y, Miyata T, Kuno A. Clinical outcomes of double-balloon endoscopy for the diagnosis and treatment of small-intestinal diseases. Clin Gastroenterol Hepatol. 2004;2:1010-1016. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 471] [Cited by in RCA: 499] [Article Influence: 23.8] [Reference Citation Analysis (0)] |
| 91. | Mönkemüller K, Weigt J, Treiber G, Kolfenbach S, Kahl S, Röcken C, Ebert M, Fry LC, Malfertheiner P. Diagnostic and therapeutic impact of double-balloon enteroscopy. Endoscopy. 2006;38:67-72. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 125] [Cited by in RCA: 134] [Article Influence: 7.1] [Reference Citation Analysis (0)] |
| 92. | Heine GD, Hadithi M, Groenen MJ, Kuipers EJ, Jacobs MA, Mulder CJ. Double-balloon enteroscopy: indications, diagnostic yield, and complications in a series of 275 patients with suspected small-bowel disease. Endoscopy. 2006;38:42-48. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 295] [Cited by in RCA: 280] [Article Influence: 14.7] [Reference Citation Analysis (0)] |
| 93. | Maconi G, Radice E, Greco S, Bianchi Porro G. Bowel ultrasound in Crohn's disease. Best Pract Res Clin Gastroenterol. 2006;20:93-112. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 84] [Cited by in RCA: 88] [Article Influence: 4.6] [Reference Citation Analysis (0)] |