Copyright
©2006 Baishideng Publishing Group Co.
World J Gastroenterol. Nov 14, 2006; 12(42): 6756-6765
Published online Nov 14, 2006. doi: 10.3748/wjg.v12.i42.6756
Published online Nov 14, 2006. doi: 10.3748/wjg.v12.i42.6756
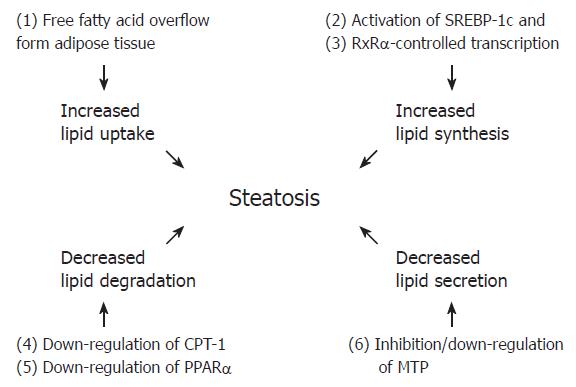
Figure 1 Some of the major mechanisms leading to steatosis in patients with chronic hepatitis C.
HCV, especially (but not only) genotype 3a, has been shown to be directly involved in triglyceride accumulation by several mechanisms: activation of fatty acid neosynthesis via SREPBP-1c (2) and RxRα (3), impaired degradation through down-regulation of CPT-1 (4) and PPARα (5), and inhibition and/or down-regulation of MTP (6). Another potential mechanism (not shown) is the cell damage inflicted by reactive oxygen species consequent to localization of the HCV core protein in the mitochondria. This may also trigger lipid peroxidation of microsomal membranes, leading to impaired VLDL secretion. In patients who are insulin resistant, the major mechanism leading to steatosis is the free fatty acid overflow from adipose tissue (1). Hyperglycemic/hyperinsulinemic states are also associated with activation of fatty acid neosynthesis via SREPBP-1c (2) and impaired degradation via down-regulation of CPT-1 (4). It has to be added that HCV may contribute to insulin resistance by impairing the IRS-1 signaling in hepatocytes by multiple mechanisms. Not shown in the figure are also the interference with ApoB synthesis and the activation of MTP reported in insulin resistant states: the latter phenomenon may be partially counterbalanced by the strong inhibition of MTP observed in patients with predominantly viral steatosis .
- Citation: Negro F. Mechanisms and significance of liver steatosis in hepatitis C virus infection. World J Gastroenterol 2006; 12(42): 6756-6765
- URL: https://www.wjgnet.com/1007-9327/full/v12/i42/6756.htm
- DOI: https://dx.doi.org/10.3748/wjg.v12.i42.6756