Copyright
©2006 Baishideng Publishing Group Co.
World J Gastroenterol. Jan 28, 2006; 12(4): 526-538
Published online Jan 28, 2006. doi: 10.3748/wjg.v12.i4.526
Published online Jan 28, 2006. doi: 10.3748/wjg.v12.i4.526
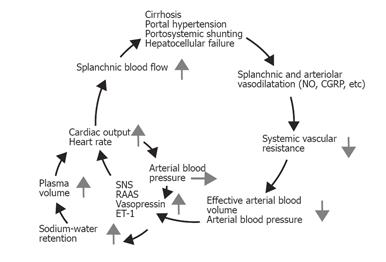
Figure 1 Pathophysiology of the splanchnic and peripheral arteriolar vasodilation and systemic hemodynamic changes in cirrhosis.
Endogenous vasodilators may escape hepatic degradation, owing to portosystemic shunting and/or hepatocellular damage, and induce vasodilatation preferentially in the splanchnic vascular area. Reduced systemic and splanchnic vascular resistance leads to a reduced effective arterial blood volume, and hence to activation of vasoconstrictor systems. The hemodynamic and clinical consequences are increases in cardiac output, heart rate, and plasma volume and decreased renal blood flow, low arterial blood pressure, and fluid and water retention. The development of the hyperdynamic circulation may increase portal inflow and further aggravate the portal pressure in a vicious cycle. SNS, sympathetic nervous system; RAAS, renin-angiotensin-aldosterone system; ET-1, endothelin-1.
- Citation: Møller S, Henriksen JH. Cardiopulmonary complications in chronic liver disease. World J Gastroenterol 2006; 12(4): 526-538
- URL: https://www.wjgnet.com/1007-9327/full/v12/i4/526.htm
- DOI: https://dx.doi.org/10.3748/wjg.v12.i4.526