Published online Jan 21, 2006. doi: 10.3748/wjg.v12.i3.489
Revised: July 28, 2005
Accepted: July 28, 2005
Published online: January 21, 2006
A 67-year old man was presented with a 6-mo history of recurrent right lower quadrant abdominal pain. On physical examination, a vague mass was palpable in the right lumbar region. His routine laboratory tests were normal. Ultrasonography showed a hypoechoic lesion in the right lumbar region anterior to the right kidney with internal echoes and fluid components. Abdominal contrast-enhanced computed tomography (CECT) showed a well-defined hypodense cystic mass lesion lateral to the ascending colon/caecum, not communicating with the lumen of colon/caecum. After complete open excision of the cystic mass lesion, gross pathologic examination revealed a turgid cystic dilatation of appendiceal remnant filled with the mucinous material. On histopathological examination, mucinous cyst adenoma of appendix was confirmed. We report this rare unusual late complication of mucocele formation in the distal viable appendiceal remnant, which was leftover following incomplete retrograde appendectomy. This unusual complication is not described in the literature and we report it in order to highlight the fact that a high index of clinical and radiological suspicion is essential for the diagnosis of mucocele arising from a distal viable appendiceal remnant in a patient who has already undergone appendectomy presenting with recurrent abdominal pain.
- Citation: Johnson MA, Jyotibasu D, Ravichandran P, Jeswanth S, Kannan DG, Surendran R. Retention mucocele of distal viable remnant tip of appendix: An unusually rare late surgical complication following incomplete appendectomy. World J Gastroenterol 2006; 12(3): 489-492
- URL: https://www.wjgnet.com/1007-9327/full/v12/i3/489.htm
- DOI: https://dx.doi.org/10.3748/wjg.v12.i3.489
Appendiceal mucocele was first described by Rokitanski in 1842[1] and an unusual variant of appendiceal mucocele -myxoglobulosis was first described by Latham in 1897[1-3].The term “mucocele of appendix”[4,5] is an inherently imprecise descriptive term that refers to any macroscopic (localised or diffuse) globular cystic dilatation of appendix (unilocular or multilocular) filled with thick tenacious mucoid/mucinous material regardless of underlying cause and is not a pathologic entity.
The majority of mucoceles of appendix arise secondary to proximal obstruction of appendiceal lumen in which the appendiceal lumen is usually in communication with caecum[6]. The potential causes of proximal appendiceal obstruction include faecolith, epithelial/mucosal hyperplasia, post inflammatory-fibrosis, cystadenoma, cystadenocarcinoma, carcinoid tumor, endometriosis and developmental anomalies such as occlusive membrane or obstructive diaphragm at the level of appendiceal orifice[7]. But the origin of mucocele of appendix from a distal viable leftover remnant tip of appendix not communicating with the caecum following incomplete retrograde open appendectomy has not been described.
We report such an extremely rare case of retention mucocele arising from a distal vascularized remnant of appendix tip, which is a leftover following incomplete open appendectomy.
We report a 67- year old man who was presented with a 6-mo history of recurrent right lower quadrant abdominal pain not associated with vomiting. He had normal appetite and bowel habits. He was not a hypertensive and diabetic, neither an alcoholic nor a smoker. He underwent open appendectomy 15 years ago. At presentation his vital parameters and systemic examination were normal. On examination of abdomen, a vague mass was palpable in the right lumbar region suspicious of a retroperitoneal tumor. Rectal examination was normal.
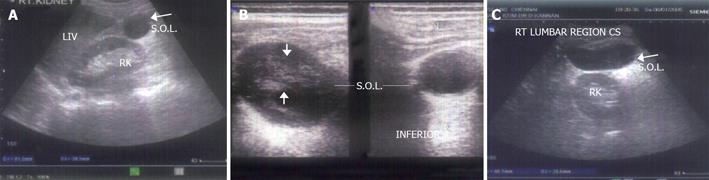
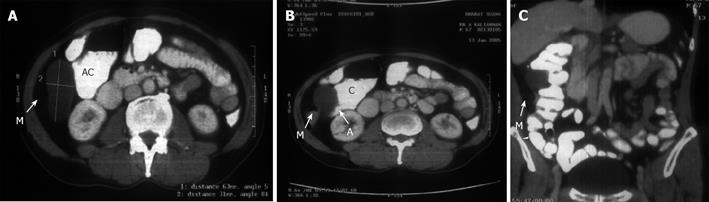
Hemoglobin value was 13.8 gm/dL(reference range: 13.5-17.0 gm/dL) and other biochemical investigations, chest X-ray and electro-cardiogram were normal. Upper gastrointestinal (GI) endoscopy and colonoscopy study was normal. Ultrasonography revealed a 6.5cm×3cm×3.5cm hypoechoic space-occupying lesion in the right lumbar region anterior to the right kidney with internal echoes and fluid components which suggested retroperitoneal cyst (Figure 1). Abdominal CECT showed a well defined blind ending tubular hypodense lesion with CT value +32 Hounsfield unit (HU) in the right lumbar region lateral to the ascending colon along the antimesenteric border (Figure 2). The lesion was not communicating with lumen of the colon, which suggested colonic duplication cyst.
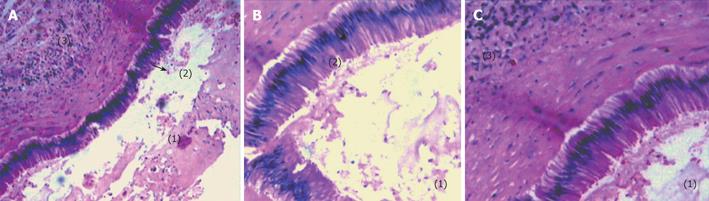
At laparotomy, a 6cm×3cm mucus-filled turgid mass was found in the distal appendiceal remnant having a separate mesentery with no communication with the ceacum (Figure 3A). Complete surgical excision was performed with an uneventful recovery. Gross pathological examination showed a distended turgid appendiceal remnant filled with characteristic mucinous material (Figures 3B, 3C). Histopathological examination showed that the appendix was lined by a single layer of mucinous epithelium with basally situated nuclei which did not show any atypia with underlying lymphoid aggregates. The appendiceal lumen showed mucinous secretions (lakes of mucin) with no epithelial elements suggestive of mucinous cyst adenoma-appendix with no evidence of malignancy or dysplasia. (Figures 4A,4B,4C). The patient was symptom-free during a 6-mo follow-up period.
Primary appendiceal mucocele, a relatively uncommon clinical entity, is most frequently an incidental finding at the time of surgery and is occasionally discovered only at pathological examination[8]. The majority of these patients are not diagnosed preoperatively and in fact 60%[8] of them are diagnosed incidentally during surgery for some other disease. The incidence of appendiceal mucocele is estimated to be 0.2-0.3% of appendicectomy specimens with myxoglobulosis constituting 0.35-0.8% of mucoceles[7].
Mucoceles are histologically subdivided into four types on the basis of World Health Organization classification[4,8].
Simple/non neoplastic mucocele or retention mucocele or obstructive form of mucocele[5] is defined as cystic dilatation of the distal appendix with accumulation of abnormal mucoid material in the appendiceal lumen secondary to appendiceal outflow obstruction.
Benign neoplastic mucocele-mucinous cystadenoma[5] is defined as dilated mucus /mucin filled appendix containing adenomatous mucosa lined by atypical mucinous epithelium containing basal nuclei and showing only minimal dysplastic features. Secondary changes[9] in mucinous cyst adenoma include thinning of the wall, extensive ulceration, calcification and ossification (“porcelain appendix”)[5]. There is also a high association between appendiceal mucinous cystadenoma with ovarian mucinous cyst adenoma and synchronous or metachronous neoplasms elsewhere in the colon[10].
Malignant mucocele[5]-mucinous cystadenocarcinoma is defined as adenocarcinoma associated with mucus-filled cystic dilatation of the appendix presenting as mucocele. A malignancy is suspected at surgery in about 30%[4-5]. In the others the diagnosis is made during pathologic examination.
Cystadenocarcinoma[4] is grossly indistinguishable from a cystadenoma. But histologically[5] the former is distinguished from mucinous cystadenoma by three criteria: presence of invasive neoplasm below the level of muscularis mucosa, when the muscularis mucosa cannot be distinguished because of distortion or fibrosis, the diagnosis is made by the finding of infiltrative tongues of tumor or single tumor cells in the wall (infiltrative appearance of border of epithelial elements) as opposed to the broad pushing edge appearance of the borders of epithelial elements that characterize mucinous tumor of uncertain/undetermined malignant potential (UMP)[5,11], presence of malignant epithelial cells in the lakes of mucin either in the wall of the appendix or outside the appendix.
Myxoglobulosis or Caviar appendix[5,7] is an extremely rare variant of appendiceal mucocele caused by proximal obstruction of appendiceal lumen in which pieces of mucinous/mucoid material can become broken off the appendiceal wall into the appendiceal lumen resulting in the formation of characteristic pearl-like translucent “mucinous globules” or pearly luminal spheroids[7] or a “cluster of frog eggs”[12] 1-10 mm in diameter with surface calcification.
Mucocele of appendix is most common in the sixth or seventh decade of life with a female preponderance[7]. The common presenting symptoms of appendiceal mucocele are episodic right lower quadrant abdominal pain (27%)[8], abdominal mass (16%)[8], weight loss (10%)[8] and change in bowel habits (5%)[8]. Complications[12-13] of mucocele include intussusception, bleeding, perforation, peritonitis, rupture and pseudomyxoma peritonei.
Colonoscopy may show a smooth glassy submucosal or extra-mucosal caecal mass moving in and out with respiratory movement. This endoscopic sign has been described as the “trapped balloon sign”[14]. The classical CT scan findings[7,15] of a mucocele in a patient who has not undergone appendectomy are a cystic low attenuation well encapsulated round or ovoid mass with smooth regular walls in the right lower quadrant adherent to caecum, mural calcification in the wall of the mucocele, and absence of peri-appendiceal inflammation or abscess which is the key differentiating point in excluding acute appendicitis. The presence of thickened wall and enhanced nodules favors the diagnosis of mucinous cystadenocarcinoma.
The clinical and radiological differential diagnosis[7,13] of mucocele of appendix includes mesenteric cyst, colonic duplication cyst, colonic lymphoma and lipoma, intussusception , right ovarian cyst and hydrosalphinx.
The treatment of mucocele of appendix is essentially by simple appendectomy but in cases of rupture or suspected malignancy a standard right hemicolectomy is indicated[8]. At the time of surgery, a spontaneous appendiceal perforation or any extravasation from appendicular lumen is strongly suggestive of malignancy in such situations, a right hemicolectomy[8,16] should always be performed with a curative intent. Laparoscopic appendectomy for mucocele removal has been described, but caution has also been suggested because of the risk of port site recurrences[17].
In a patient who has undergone open appendectomy, with the CT finding of a cystic well encapsulated mass in the right lumbar region adherent to the pulled up caecum/ascending colon not communicating with the lumen of colon/caecum, one should consider the possibility of mucocele of distal appendiceal remnant. Therefore, a high index of clinical and radiological suspicion is essential for the preoperative diagnosis of mucocele of distal appendiceal remnant in a patient who has undergone appendectomy.Incomplete surgical removal of appendix must be avoided in order to prevent the late complication of mucocele formation in the distal leftover vascularized remnant tip of appendix. All appendiceal mucoceles measuring at least 2 cm must be completely excised to eliminate the chance of progression to malignancy. The association between appendiceal mucocele and colonic neoplasm is more clear and logical to recommend surveillance colonoscopy in patients with diagnosis of appendiceal mucocele, at least in those with appendiceal mucinous cystadenoma.
S- Editor Wang XL and Guo SY L- Editor Elsevier HK E- Editor Liu WF
| 1. | Gonzalez JE, Hann SE, Trujillo YP. Myxoglobulosis of the appendix. Am J Surg Pathol. 1988;12:962-966. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 27] [Cited by in RCA: 28] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 2. | Lubin J, Berle E. Myxoglobulosis of the appendix. Report of two cases. Arch Pathol. 1972;94:533-536. [PubMed] |
| 4. | Appelman HD. Epithelial neoplasia of the appendix. Pathology of the colon, small intestine, and anus 2nd ed. New York: Churchill Livingstone pub 1991; 263-303. |
| 5. | Parakrama Chandrasoma. Gastrointestinal Pathology. 1st ed. Appleton& Lange pub. New York: Churchill Livingstone pub 1999; 239-241. |
| 6. | Stacey E. Mills. Sternberg’s Diagnostic Surgical Pathology. 4th ed. Lippincott Willams/Wilkins pub. New York: Churchill Livingstone pub 2004; 1576-1599. |
| 7. | Viswanath YK, Griffiths CD, Shipsey D, Oriolowo A, Johnson SJ. Myxoglobulosis, a rare variant of appendiceal mucocele, occurring secondary to an occlusive membrane. J R Coll Surg Edinb. 1998;43:204-206. [PubMed] |
| 8. | Stocchi L, Wolff BG, Larson DR, Harrington JR. Surgical treatment of appendiceal mucocele. Arch Surg. 2003;138:585-59; discussion 585-59;. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 107] [Cited by in RCA: 110] [Article Influence: 5.0] [Reference Citation Analysis (0)] |
| 9. | Juan Rosai – Rosai and Ackerman’s Surgical pathology. 9th ed. Vol I. Mosby pub. New York: Churchill Livingstone pub 2004; 761– 765. |
| 10. | Seidman JD, Elsayed AM, Sobin LH, Tavassoli FA. Association of mucinous tumors of the ovary and appendix. A clinicopathologic study of 25 cases. Am J Surg Pathol. 1993;17:22-34. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 108] [Cited by in RCA: 113] [Article Influence: 3.5] [Reference Citation Analysis (0)] |
| 11. | Isaacs KL, Warshauer DM. Mucocele of the appendix: computed tomographic, endoscopic, and pathologic correlation. Am J Gastroenterol. 1992;87:787-789. [PubMed] |
| 12. | Dachman AH, Lichtenstein JE, Friedman AC. Mucocele of the appendix and pseudomyxoma peritonei. AJR Am J Roentgenol. 1985;144:923-929. [PubMed] |
| 13. | Huang HC, Liu TP, Jeng KS. Intussusception of mucocele of the appendix: a case report. Zhonghua Yi Xue Za Zhi (Taipei). 1994;53:120-123. [PubMed] |
| 14. | Raijman I, Leong S, Hassaram S, Marcon NE. Appendiceal mucocele: endoscopic appearance. Endoscopy. 1994;26:326-328. [PubMed] |
| 15. | Zissin R, Gayer G, Kots E, Apter S, Peri M, Shapiro-Feinberg M. Imaging of mucocoele of the appendix with emphasis on the CT findings: a report of 10 cases. Clin Radiol. 1999;54:826-832. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 49] [Cited by in RCA: 47] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 16. | Nitecki SS, Wolff BG, Schlinkert R, Sarr MG. The natural history of surgically treated primary adenocarcinoma of the appendix. Ann Surg. 1994;219:51-57. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 217] [Cited by in RCA: 207] [Article Influence: 6.7] [Reference Citation Analysis (0)] |
| 17. | González Moreno S, Shmookler BM, Sugarbaker PH. Appendiceal mucocele. Contraindication to laparoscopic appendectomy. Surg Endosc. 1998;12:1177-1179. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 86] [Cited by in RCA: 78] [Article Influence: 2.9] [Reference Citation Analysis (0)] |