Copyright
©2006 Baishideng Publishing Group Co.
World J Gastroenterol. Jun 14, 2006; 12(22): 3512-3522
Published online Jun 14, 2006. doi: 10.3748/wjg.v12.i22.3512
Published online Jun 14, 2006. doi: 10.3748/wjg.v12.i22.3512
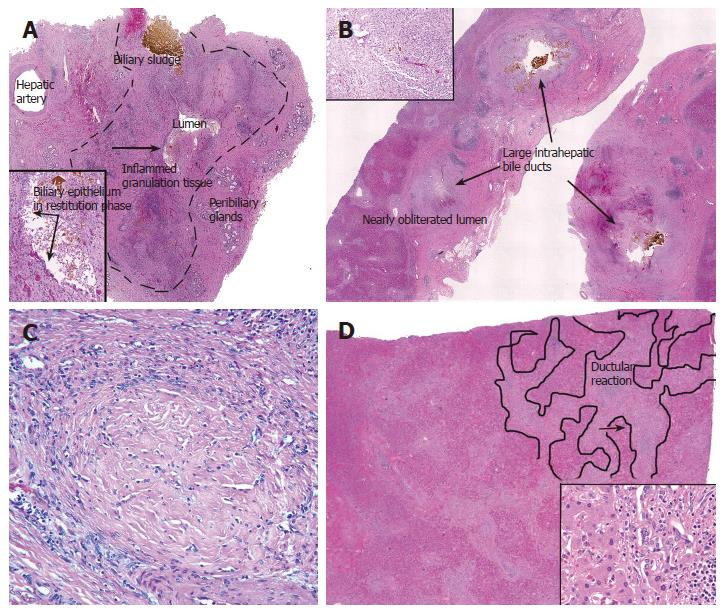
Figure 2 A: Cross-section of an extra-hepatic bile duct (outlined by dashed lines) from a liver allograft that failed because of the biliary sludge syndrome.
Note the hepatic artery branch traveling along the outer wall, the peribiliary glands, mucosal ulceration, and that the lumen is nearly obliterated. Ulceration exposes the underlying stroma to bile, which results in inflammation, granulation tissue, and myofibroblast activation and proliferation in the underlying stroma. The inset shows at higher magnification the area near the arrow; note the bile sludge, BEC in restitution phase, and stromal inflammation and granulation tissue (arrows); B: Cross-section of several large intra-hepatic bile ducts from the same liver. Note that the same processes are occurring in these ducts. The duct lumen in the lower left is nearly obliterated by inflamed granulation tissue and myofibroblasts (inset); C: The final stages of “pathologic wound healing” in the intra-hepatic ducts can result in complete fibrous obliteration of the bile duct lumen by concentric rings of fibrous tissue, as shown here; D: Sections from the periphery of the same liver show a prominent ductular reaction consisting of BEC and periductal myofibroblasts (inset). This occurs because of increased pressure in the biliary tree distal to the site of luminal obliteration. Notice that the cholangioles and myofibroblasts form a wedge of tissue that arises from the portal tract and distorts the liver architecture (outlined on the right side of image).
- Citation: Demetris AJ, III JGL, Specht S, Nozaki I. Biliary wound healing, ductular reactions, and IL-6/gp130 signaling in the development of liver disease. World J Gastroenterol 2006; 12(22): 3512-3522
- URL: https://www.wjgnet.com/1007-9327/full/v12/i22/3512.htm
- DOI: https://dx.doi.org/10.3748/wjg.v12.i22.3512