Published online Feb 7, 2005. doi: 10.3748/wjg.v11.i5.748
Revised: April 12, 2004
Accepted: May 13, 2004
Published online: February 7, 2005
AIM: To evaluate the patterns with metastasis of gallbladder carcinoma in lymph nodes and liver.
METHODS: A total of 45 patients who had radical surgery were selected. The patterns with metastasis of primary gallbladder carcinoma in lymph nodes and liver were examined histopathologically and classified as TNM staging of the American Joint Committee on Cancer.
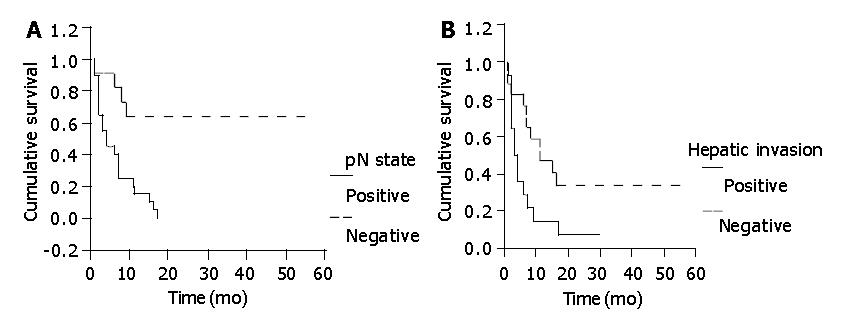
RESULTS: Of the 45 patients, 29 (64.4%) had a lymph node positive disease and 20 (44.4%) had a direct invasion of the liver. The frequency of involvement of lymph nodes was strongly influenced by the depth of the primary tumor (P = 0.0001). The postoperative survival rate of patients with negative lymph node metastasis was significantly higher than that of patients with positive lymph node metastasis (P = 0.004), but the postoperative survival rate of patients with N1 lymph node metastasis was not significantly different from that of patients with N2 lymph node metastasis (P = 0.3874). The postoperative survival rate of patients without hepatic invasion was significantly better than that of patients with hepatic invasion (P = 0.0177).
CONCLUSION: Complete resection of the regional lymph nodes is important in advanced primary gallbladder carcinoma (PGC). The initial sites of liver spread are located mostly in segments IV and V. It is necessary to achieve negative surgical margins 2 cm from the tumor. In patients with hepatic hilum invasion, extended right hepatectomy with or without bile duct resection or portal vein resection is necessary for curative resection.
- Citation: Lin HT, Liu GJ, Wu D, Lou JY. Metastasis of primary gallbladder carcinoma in lymph node and liver. World J Gastroenterol 2005; 11(5): 748-751
- URL: https://www.wjgnet.com/1007-9327/full/v11/i5/748.htm
- DOI: https://dx.doi.org/10.3748/wjg.v11.i5.748
Primary gallbladder carcinoma (PGC) is one of the most common malignancies of the biliary tract with poor prognosis[1,2], because it is usually detected at an advanced stage due to no specific symptoms[3]. The only potentially curative therapy for gallbladder carcinoma is surgical resection. The spread modes of gallbladder carcinoma are direct, lymphatic, vascular, neural, intraperitoneal, and intraductal. Liver and lymph nodes are the two most common sites of metastasis of gallbladder carcinoma[4,5]. The purpose of the present study was to assess the spread patterns of gallbladder carcinoma and to discuss the related radical resection methods.
From April 1994 to October 2003, a total of 138 patients with primary gallbladder carcinoma were treated in our hospital. Patients without surgery (n = 36) and patients with palliative surgery (n = 57) were excluded from the study. Forty-five patients undergone radical surgery were included in this study, 22 were men and 23 women, with a mean age of 61.22 years (range: 33-85 years).
Radical resection was defined as the complete removal of a regional tumor with free surgical margins and positive lymph node metastasis restricted to the dissected area, as seen on postoperative histological examination.
The operative procedures are shown in Table 1. Simple cholecystectomy was performed in 3 patients, other patients underwent lymphadenectomy. The operative procedures included wedge resection (n = 8), resection of segments IV a and V (n = 20), resection of the bile duct (n = 8), extended right hepatectomy (n = 2), hepatopancreaticoduodenectomy (n = 5), and other organ tissue resection (n = 6), portal vein resection (n = 2), proper hepatic artery resection (n = 1). The resected specimens were examined histopathologically. Hepatic and lymph node specimens were especially concerned. The TNM system of the American Joint Committee on Cancer (AJCC) was used for staging.
| Type of resection | Patients (n) | Percent (%) | I | II | III | IV A | IV B |
| C | 3 | 6.7 | 2 | 1 | |||
| C+N | 7 | 15.6 | 2 | 3 | 2 | ||
| C+WR+N | 8 | 17.8 | 1 | 2 | 2 | 1 | 2 |
| C+S4aS5+N | 6 | 13.3 | 4 | 2 | |||
| C+S4aS5+BD+N | 8 | 17.8 | 5 | 3 | |||
| C+ERH+N | 2 | 4.4 | 1 | 1 | |||
| HPD+N | 5 | 11.1 | 1 | 4 | |||
| C+S4aS5+Other+N | 6 | 13.3 | 1 | 2 | 3 | ||
| Total | 45 | 100 | 5 | 6 | 5 | 14 | 15 |
Cumulative survival rate was determined with the Kaplan-Meier method. Differences in the survival curves were compared with the Log-rank test. P<0.05 was considered statistically significant.
The 29 patients (64.4%) with a lymph node-positive disease had N1 (n = 15) and N2 (n = 14) stages of primary gallbladder carcinoma. Of these patients, 7 had positive cystic nodes, 22 had positive pericholedochal nodes, 10 had positive hepatic hilum nodes, 2 had positive retroportal nodes, 3 had positive nodes along the common hepatic artery, 12 had positive postersuperior pancreaticoduodenal nodes, 1 had positive celiac nodes, 1 had positive superior mesenteric nodes, 3 had positive nodes at the greater curvature of the stomach, 4 had positive para-aortic nodes. All patients with positive para-aortic nodes had N2 stage of primary gallbladder carcinoma. The relationship between N stage and T stage is shown in Table 2. The frequency of lymph node involvement was strongly influenced by the invasion depth of the primary tumor (P = 0.0001).
| Depth of tumor | No. of patients with lymph node metastasis | |||
| N0 | N1 | N2 | Para-aortic lymph node | |
| T1 (n = 6) | 5 | 1 | 0 | 0 |
| T2 (n = 8) | 6 | 1 | 1 | 1 |
| T3 (n = 5) | 1 | 2 | 2 | 0 |
| T4 (n = 26) | 4 | 11 | 11 | 3 |
| Total (n = 45) | 16 | 15 | 14 | 4 |
Primary lesions were located in the fundus (n = 14), body(n = 12), neck (n = 7), both in the fundus and in the body (n = 2), both in the fundus and in the neck (n = 2) of the gallbladder, and in the whole gallbladder (n = 8). In 31 patients, the primary lesions were extended out of the gallbladder into the surrounding tissues.
Tumors of gallbladder invaded into the liver (n = 20), segment IV (n = 1), segment V (n = 2), segments IV and V (n = 15), segments IV, V and VIII (n = 2). Tumors invaded into the bile duct (n = 12). There were 3 cases in the third stage. Locations of tumors were in the pancreatic head (n = 4), nerve (n = 3), portal vein (n = 2), proper hepatic artery (n = 1), duodenum (n = 3) and right transverse colon invasion (n = 2).
There were 2 patients with right hepatic metastasis, 2 with abdominal peritoneum metastasis, 1 with ileum metastasis. All metastasitic lesions were completely resected.
Based on AJCC TNM staging system, the distributions were in T1 (n = 6), T2 (n = 8), T3 (n = 5), T4 (n = 26), N0 (n = 16), N1 (n = 15), N2 (n = 14), M0 (n = 39), M1 (n = 6). Five cases were stage I, six cases stage II, five cases stage III, fourteen cases stage IVA, and fifteen cases stage IVB.
Three cases died in hospital of postoperative hepatic failure. Postoperative morbidity and mortality rates of 45 patients were 33.3% and 6.7%, respectively. A total of 31 patients were followed up. Postoperative survival rate was poor in our series as compared to others, with an 1-year survival rate of 32.3% and 3-year survival rate of 9.7%. The postoperative survival rate of patients without lymph node metastasis was significantly better than that of patients with lymph node metastasis (P = 0.004, Figure 1A), but the postoperative survival rate of patients with N1 lymph node metastasis was not significantly different from that of patients with N2 lymph node metastasis (P = 0.3874). The postoperative survival rate of patients without hepatic invasion was significantly better than that of patients with hepatic invasion (P = 0.0177, Figure 1B).
The prognosis of patients with gallbladder carcinoma remains dismal especially in advanced cases. The role of surgery in the treatment of gallbladder carcinoma is still controversial. The pattern and outcome of prospective radical surgery depend on the mode and degree of tumor spread[6].
Shirai et al[7] reported that gallbladder lymph circulated though the pericholedochal lymph nodes to the posterosuperior pancreaticoduodenal lymph nodes, and interaoticoval lymph nodes. Ito et al[8] have proposed three pathways of lymphatic drainage from the gallbladder: the cholecystoretropancreatic pathway, the cholecystoceliac pathway and the cholecystomesenteric pathway. But this does not concern the modes of flows to the hepatic hilum lymph nodes. This study also shows that the hepatic hilum lymph node metastasis is a common lymph node metastasis position (10 patients, 34.5%). The cystic and pericholedochal lymph nodes are the initial spreading sites from PBC.
The prognosis of PGC is strongly affected by their lymph node status[9,10]. Some authors indicate that there is no difference in survival between N0 and N1 patients, while patients with a N2 disease have a significantly worse prognosis[11]. Some authors indicate that there is no difference in survival between N1 and N2 patients, while patients with a N0 disease have a significantly better prognosis[12]. This study shows that N0 patients have a significantly better survival than N1 patients, but there is no difference in survival between N1 and N2 patients. The different conclusions maybe due to the different radical procedures. After a complete resection of the posterosuperior pancreaticoduodenal nodes, superior mesenteric nodes and celiac nodes, even para-aortic lymph nodes, N2 patients could get a survival rate as N1 patients.
Conflicting radical resection of lymph node metastasis was reported. Benoist et al[1] advocate that radical resection should only be considered in the absence of regional lymph node metastasis, while Chijiiwa et al[9] believe that radical resection should be done for patients with involvement confined to the hepatoduodenal ligaments, posterosuperior pancreaticoduodenal area, and the common hepatic artery, but do not advocate radical resection for patients with superior mesenteric node, celiac node, and para-aortic lymph node metastases. Tsukada et al[11] suggest a more extensive dissection even with pancreaticoduodenectomy and resection of the para-aortic lymph nodes in selected patients. This study also shows that N2 patients with a more extensive dissection could get a better prognosis than N1 patients.
Some authors advocate that there is no lymph node metastasis in T1 patients[11,13,14]. One T1 patient had pN1 lymph node metastasis (the primary lesion invaded muscle layer) (Table 2), 1 patient had N1 lymph node metastasis and 1 had both N2 and para-aortic lymph node metastases in T2 patients. Complete removal of regional lymph nodes is important in advanced PGC, only patients with tumor lesions lying in mucosae could be treated with simply cholecystectomy[15]. Radical resection is comprised of resection of the lymph nodes around the head of pancreas, including the lymph nodes along the common hepatic artery, celiac nodes, retroportal lymph nodes, and para-aortic lymph nodes in the aorticocaval space[16]. A sampling biopsy of para-aortic nodes may be useful before starting a radical resection[17]. If hepatic hilum lymph nodes are positive, resection of segments IV a and V would be necessary to prevent lymphatic hepatic metastasis[18].
Shirai et al[19] reported three patterns of direct hepatic invasion. Some authors indicate that venous blood from the gallbladder is drained into segments IV and V by short direct communicating veins or by veins accompanying the extrahepatic ducts into the liver[20]. This explains why the initial location of liver metastasis is to the portions adjacent to the gallbladder, mostly in segments IV and V, rather than the distant sites of the liver. According to Yoshimitsu et al[21], 96% of gallbladder veins end in the intrahepatic portal branches of segment V, 93% of gallbladder veins end in the intrahepatic portal branches of segment IV. The portal tract lymphatic retrograde spread may be a reason of gallbladder metastasis. This study shows that the most common hepatic spread position is segments IV and V (15 patients, 75%).
Ogura et al[22] reported two patterns of hepatic infiltration, the extensive pattern and the infiltrating pattern. Two modes of tumor invasion have been noted in the infiltrating pattern, the most common site of the main tumor is located in hepatic parenchyma, the front of carcinoma involving vascular infiltration invades the hepatic hilum along the Glisson’s sheath. Localized hepatic metastases from gallbladder carcinoma near the gallbladder bed are also reported[19]. The most important route of early hepatic metastasis from gallbladder carcinoma seems to be the portal tracts[23].
Hepatic resection for advanced carcinoma of the gallbladder must be decided on the basis of the modes of tumor spread to the liver. Wedge resection or resection of segments IV a and V should be considered as an adequate hepatectomy for patients with subserosal invasion[24,25], because early metastasis foci have been detected not only in patients with direct invasion of the liver but also in those without direct invasion. Various degrees of hepatic resection are needed to comply with the depth of direct invasion. It is necessary to achieve negative surgical margins 2 cm from the tumor. In patients with hepatic hilum invasion, extended right hepatectomy with or without bile duct resection or portal vein resection would be necessary for curative resection because the front of carcinoma invasion along the Glisson’s sheath is often longer than the extensive pattern tumors. A caudate lobectomy is often needed for this type of radical resection[22,26]. Central bisegmentectomy plus caudate lobectomy is a useful procedure for infiltrating type of gallbladder carcinoma[27].
In conclusion, complete excision of regional lymph nodes is important in advanced PGC, only patients with tumors lying in mucosae can be treated with simpl cholecystectomy. In patients with hepatic hilum invasion, extended right hepatectomy with or without bile duct resection or portal vein resection is necessary for curative resection.
Edited by Wang XL and Ren SR
| 1. | Benoist S, Panis Y, Fagniez PL. Long-term results after curative resection for carcinoma of the gallbladder. French University Association for Surgical Research. Am J Surg. 1998;175:118-122. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 135] [Cited by in F6Publishing: 147] [Article Influence: 5.7] [Reference Citation Analysis (0)] |
| 2. | Ishikawa T, Horimi T, Shima Y, Okabayashi T, Nishioka Y, Hamada M, Ichikawa J, Tsuji A, Takamatsu M, Morita S. Evaluation of aggressive surgical treatment for advanced carcinoma of the gallbladder. J Hepatobiliary Pancreat Surg. 2003;10:233-238. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 37] [Cited by in F6Publishing: 33] [Article Influence: 1.7] [Reference Citation Analysis (0)] |
| 3. | Donohue JH. Present status of the diagnosis and treatment of gallbladder carcinoma. J Hepatobiliary Pancreat Surg. 2001;8:530-534. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 68] [Cited by in F6Publishing: 71] [Article Influence: 3.2] [Reference Citation Analysis (0)] |
| 4. | Kokudo N, Makuuchi M, Natori T, Sakamoto Y, Yamamoto J, Seki M, Noie T, Sugawara Y, Imamura H, Asahara S. Strategies for surgical treatment of gallbladder carcinoma based on information available before resection. Arch Surg. 2003;138:741-750; discussion 750. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 99] [Cited by in F6Publishing: 101] [Article Influence: 4.8] [Reference Citation Analysis (0)] |
| 5. | Ohtani T, Shirai Y, Tsukada K, Muto T, Hatakeyama K. Spread of gallbladder carcinoma: CT evaluation with pathologic correlation. Abdom Imaging. 1996;21:195-201. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 78] [Cited by in F6Publishing: 79] [Article Influence: 2.8] [Reference Citation Analysis (0)] |
| 6. | Noshiro H, Chijiiwa K, Yamaguchi K, Shimizu S, Sugitani A, Tanaka M. Factors affecting surgical outcome for gallbladder carcinoma. Hepatogastroenterology. 2003;50:939-944. [PubMed] [Cited in This Article: ] |
| 7. | Shirai Y, Yoshida K, Tsukada K, Ohtani T, Muto T. Identification of the regional lymphatic system of the gallbladder by vital staining. Br J Surg. 1992;79:659-662. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 90] [Cited by in F6Publishing: 67] [Article Influence: 2.1] [Reference Citation Analysis (1)] |
| 8. | Ito M, Mishima Y, Sato T. An anatomical study of the lymphatic drainage of the gallbladder. Surg Radiol Anat. 1991;13:89-104. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 64] [Cited by in F6Publishing: 63] [Article Influence: 1.9] [Reference Citation Analysis (0)] |
| 9. | Chijiiwa K, Noshiro H, Nakano K, Okido M, Sugitani A, Yamaguchi K, Tanaka M. Role of surgery for gallbladder carcinoma with special reference to lymph node metastasis and stage using western and Japanese classification systems. World J Surg. 2000;24:1271-126; discussion 1277. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 53] [Cited by in F6Publishing: 57] [Article Influence: 2.4] [Reference Citation Analysis (0)] |
| 10. | Shimada H, Endo I, Togo S, Nakano A, Izumi T, Nakagawara G. The role of lymph node dissection in the treatment of gallbladder carcinoma. Cancer. 1997;79:892-899. [PubMed] [DOI] [Cited in This Article: ] [Cited by in F6Publishing: 3] [Reference Citation Analysis (0)] |
| 11. | Tsukada K, Kurosaki I, Uchida K, Shirai Y, Oohashi Y, Yokoyama N, Watanabe H, Hatakeyama K. Lymph node spread from carcinoma of the gallbladder. Cancer. 1997;80:661-667. [PubMed] [DOI] [Cited in This Article: ] [Cited by in F6Publishing: 2] [Reference Citation Analysis (0)] |
| 12. | Shimada H, Endo I, Fujii Y, Kamiya N, Masunari H, Kunihiro O, Tanaka K, Misuta K, Togo S. Appraisal of surgical resection of gallbladder cancer with special reference to lymph node dissection. Langenbecks Arch Surg. 2000;385:509-514. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 39] [Cited by in F6Publishing: 39] [Article Influence: 1.6] [Reference Citation Analysis (0)] |
| 13. | Wakai T, Shirai Y, Yokoyama N, Nagakura S, Watanabe H, Hatakeyama K. Early gallbladder carcinoma does not warrant radical resection. Br J Surg. 2001;88:675-678. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 123] [Cited by in F6Publishing: 135] [Article Influence: 5.9] [Reference Citation Analysis (0)] |
| 14. | Toyonaga T, Chijiiwa K, Nakano K, Noshiro H, Yamaguchi K, Sada M, Terasaka R, Konomi K, Nishikata F, Tanaka M. Completion radical surgery after cholecystectomy for accidentally undiagnosed gallbladder carcinoma. World J Surg. 2003;27:266-271. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 89] [Cited by in F6Publishing: 82] [Article Influence: 3.9] [Reference Citation Analysis (0)] |
| 15. | Wagholikar GD, Behari A, Krishnani N, Kumar A, Sikora SS, Saxena R, Kapoor VK. Early gallbladder cancer. J Am Coll Surg. 2002;194:137-141. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 66] [Cited by in F6Publishing: 72] [Article Influence: 3.3] [Reference Citation Analysis (0)] |
| 16. | Noie T, Kubota K, Abe H, Kimura W, Harihara Y, Takayama T, Makuuchi M. Proposal on the extent of lymph node dissection for gallbladder carcinoma. Hepatogastroenterology. 1999;46:2122-2127. [PubMed] [Cited in This Article: ] |
| 17. | Kondo S, Nimura Y, Hayakawa N, Kamiya J, Nagino M, Uesaka K. Regional and para-aortic lymphadenectomy in radical surgery for advanced gallbladder carcinoma. Br J Surg. 2000;87:418-422. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 167] [Cited by in F6Publishing: 171] [Article Influence: 7.1] [Reference Citation Analysis (0)] |
| 18. | Uesaka K, Yasui K, Morimoto T, Torii A, Yamamura Y, Kodera Y, Hirai T, Kato T, Kito T. Visualization of routes of lymphatic drainage of the gallbladder with a carbon particle suspension. J Am Coll Surg. 1996;183:345-350. [PubMed] [Cited in This Article: ] |
| 19. | Shirai Y, Tsukada K, Ohtani T, Watanabe H, Hatakeyama K. Hepatic metastases from carcinoma of the gallbladder. Cancer. 1995;75:2063-2068. [PubMed] [DOI] [Cited in This Article: ] [Cited by in F6Publishing: 1] [Reference Citation Analysis (0)] |
| 20. | Boerma EJ. Towards an oncological resection of gall bladder cancer. Eur J Surg Oncol. 1994;20:537-544. [PubMed] [Cited in This Article: ] |
| 21. | Yoshimitsu K, Honda H, Kaneko K, Kuroiwa T, Irie H, Chijiiwa K, Takenaka K, Masuda K. Anatomy and clinical importance of cholecystic venous drainage: helical CT observations during injection of contrast medium into the cholecystic artery. AJR Am J Roentgenol. 1997;169:505-510. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 70] [Cited by in F6Publishing: 69] [Article Influence: 2.6] [Reference Citation Analysis (0)] |
| 22. | Ogura Y, Tabata M, Kawarada Y, Mizumoto R. Effect of hepatic invasion on the choice of hepatic resection for advanced carcinoma of the gallbladder: histologic analysis of 32 surgical cases. World J Surg. 1998;22:262-266; discussion 266-267. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 31] [Cited by in F6Publishing: 34] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 23. | Ohtsuka M, Miyazaki M, Itoh H, Nakagawa K, Ambiru S, Shimizu H, Nakajima N, Akikusa B, Kondo Y. Routes of hepatic metastasis of gallbladder carcinoma. Am J Clin Pathol. 1998;109:62-68. [PubMed] [Cited in This Article: ] |
| 24. | Suzuki S, Yokoi Y, Kurachi K, Inaba K, Ota S, Azuma M, Konno H, Baba S, Nakamura S. Appraisal of surgical treatment for pT2 gallbladder carcinomas. World J Surg. 2004;28:160-165. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 60] [Cited by in F6Publishing: 52] [Article Influence: 2.6] [Reference Citation Analysis (0)] |
| 25. | Chijiiwa K, Nakano K, Ueda J, Noshiro H, Nagai E, Yamaguchi K, Tanaka M. Surgical treatment of patients with T2 gallbladder carcinoma invading the subserosal layer. J Am Coll Surg. 2001;192:600-607. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 130] [Cited by in F6Publishing: 123] [Article Influence: 5.3] [Reference Citation Analysis (0)] |
| 26. | Kondo S, Nimura Y, Kamiya J, Nagino M, Kanai M, Uesaka K, Hayakawa N. Mode of tumor spread and surgical strategy in gallbladder carcinoma. Langenbecks Arch Surg. 2002;387:222-228. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 62] [Cited by in F6Publishing: 66] [Article Influence: 3.0] [Reference Citation Analysis (0)] |
| 27. | Ogura Y, Matsuda S, Sakurai H, Kawarada Y, Mizumoto R. Central bisegmentectomy of the liver plus caudate lobectomy for carcinoma of the gallbladder. Dig Surg. 1998;15:218-223. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 23] [Cited by in F6Publishing: 23] [Article Influence: 1.0] [Reference Citation Analysis (0)] |