Published online Aug 14, 2005. doi: 10.3748/wjg.v11.i30.4761
Revised: January 1, 2005
Accepted: January 5, 2005
Published online: August 14, 2005
Mucocele of the appendix is a rare lesion, characterized by distension of the lumen due to accumulation of mucoid substance. This disease is often asymptomatic and pre-operative diagnosis is rare. If untreated, one type of mucocele may rupture producing a potentially fatal entity known as pseudomyxoma peritonei. The type of surgical treatment is related to the dimensions and to histology of the mucocele. Appendectomy is used for simple mucocele or for cystadenoma. Right hemi-colectomy is recommended for cystadenocarcinoma. In this paper, we report a case of a 51-year-old woman with a mobile, painless mass in the right lower quadrant of abdomen caused by a giant appendiceal mucocele. Imaging showed a large, tubular, cystic structure extending below from the inferior wall of the cecum. Surgery revealed a giant retro-cecal appendix measuring 17 cm in length and 4 cm in diameter. The final pathologic diagnosis was mucocele caused by mucinous cystadenoma.
- Citation: Rampone B, Roviello F, Marrelli D, Pinto E. Giant appendiceal mucocele: Report of a case and brief review. World J Gastroenterol 2005; 11(30): 4761-4763
- URL: https://www.wjgnet.com/1007-9327/full/v11/i30/4761.htm
- DOI: https://dx.doi.org/10.3748/wjg.v11.i30.4761
Mucocele is a rare pathology of the appendix, characterized by a cystic dilation of the lumen with stasis of mucus. The incidence ranges between 0.2% and 0.3% of all appendectomies, with a higher frequency in females (4/1) and in people more than 50 years[1]. It demonstrates an inflammatory or a tumoral cause; most important for the surgeon, however, the mucoceles are caused by mucinous cystadenomas and cystadenoca-rcinomas. In the latter case, a possible rupture of the mucocele, either spontaneous or accidental, may result in the clinical condition of pseudomyxoma peritonei, a spread of malignant cells throughout the peritoneal cavity in the form of multiple mucinous deposits[2,3]. A correct diagnosis may help to avoid iatrogenic rupture during surgery. We describe a case of a giant appendiceal mucocele and present the diagnostic aspects, surgical options and prognosis of this disease.
A 51-year-old woman was admitted to our department on April 21, 2004 due to the appearance of a mass in the right lower quadrant of abdomen, with nausea and decreased appetite. No urinary dysfunction or changes in her intestinal transit was reported. Her blood pressure was 130/80 mmHg with regular pulse of 80/min. She had a body temperature of 36.8°C. On admission, physical examination of chest revealed no abnormalities and superficial lymph nodes were not palpable. A mobile, painless mass was palpated at the right lower abdomen. No liver or spleen enlargements were noted.
Laboratory tests, including CEA, CA 19-9, CA 125, CA 15-3 and CA 72-4, were unremarkable.
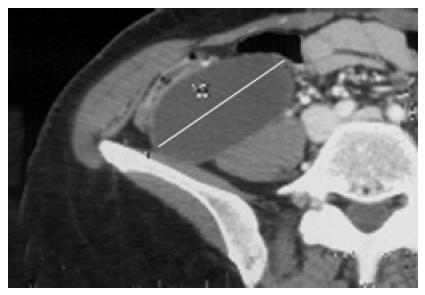
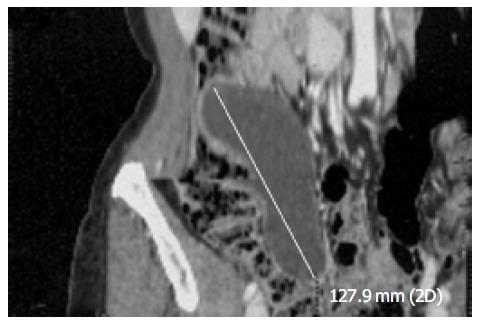
Abdominal ultrasonography revealed the presence of a non-homogeneous oval mass. Computed tomography scan of the abdomen showed a large, hypodense, tubular, cystic structure extending below the inferior wall of the cecum (Figure 1). Coronal view of computed tomography disclosed a mass, which measured about 13 cm in length (Figure 2).
On April 24 the patient had a laparotomy. At surgery, a giant retro-cecal appendix was found (Figure 3). There was no lymphadenopathy or hepatic metastases. No other tumors were noted in the abdominal or pelvic cavities. The appendix was bent behind the ascending colon. After adhesiotomy, a standard appendectomy was performed.
The mass, which measured 17 cm in length and 4 cm in diameter, showed a thin fibrous wall and viscous hemorrhagic mucoid content without any mucosal lesion. The final pathologic diagnosis was mucocele caused by mucinous cystadenoma. There was no evidence of malignancy. The patient’s post-operative course was unremarkable and she was discharged 5 d post-operatively.
At present, about 7 mo post-operatively, the patient is asymptomatic, and abdominal ultrasonography did not reveal any abdominal lesion.
The term mucocele is often used as a general descriptive term for dilatation of the appendiceal lumen by mucinous secretions. Four subgroups of the disease can be identified, according to the characteristics of the epithelium: (1) simple or retention mucoceles resulting from obstruction of the appendiceal outflow, usually by a fecalith, and characterized by normal epithelium and mild luminal dilatation up to 1 cm. (2)Mucoceles with hyperplastic epithelium where luminal dilatation is also mild; these constitute 5-25% of mucoceles.
Benign mucoceles, the most common form, accounting for 63-84% of cases. These exhibit mostly epithelial villous adenomatous changes with some degree of epithelial atypia, and are characterized by marked distention of the lumen up to 6 cm. Our patient belongs to this group. (4) Malignant mucinous cystadenocarcinomas, representing 11-20% of cases. They are distinguished from the previous group by their glandular stromal invasion and/or presence of epithelial cells in the peritoneal implants. The luminal distention is usually severe[1-4].
Mucinous cystadenomas and cystadenocarcinomas are often referred to as neoplastic mucoceles. In cystadenomas, which are the most common form, the luminal dilatation reaches up to 6 cm and is associated with appendiceal perforation in 20% of instances. This results in mucinous spillage into the peri-appendicular area and peritoneal cavity. Histological examination of the mucus does not reveal any neoplastic cells and appendectomy is usually curative[5]. Mucinous cystaden-ocarcinomas, on the other hand, are less common than mucinous cystadenomas and may present with spontaneous rupture in 6% of cases. Macroscopically, they produce mucin-filled cystic dilatation of the appendix indistinguishable from cystadenomas. However, neoplastic cells may penetrate the appendiceal wall and spread beyond the appendix in the form of peritoneal implants. In its fully developed state, the peritoneal cavity becomes distended with adhesive, semi-solid mucin in which neoplastic adenocarcinomatous cells can be found; this condition is termed as pseudomyxoma peritonei. The intraperitoneal spread of this mucin-secreting cancer is identical to that of intra-peritoneal ovarian mucinous cystadenocarcinomas[2-5].
Symptomatology of appendiceal mucoceles is not specific: very large lesions are asymptomatic in 25% of patients. The most common presentation is right lower quadrant pain, similar to an acute appendicitis; a palpable mass can be found in 50% of cases, whereas urinary dysfunction or hematuria is rarely related[6]. Increase of tumor markers indicate a probable neoplastic origin[7,8]. The rare complications include intestinal obstruction, frequently caused by intussu-sception, or intestinal bleeding. Pseudomyxoma is the worst complication, characterized by peritoneal dissemination caused by spontaneous or iatrogenic perforation of the appendix. In benign mucocele, the pseudomyxoma is confined to the peri-appendicular area. In malignant cases, this dissemination is considered a real metastatic entity; retro-peritoneal or pleural implants are occasionally reported[7-9].
Preoperative diagnosis is difficult, due to the nonspecific nature of the disease. The lesion may be identified by radiologic, sonographic, or endoscopic means. Elevated carcino-embryonic antigen levels have been described in neoplastic mucoceles[10,11].
Computed tomography scan of the abdomen is important in the diagnosis and evaluation of the extent of the disease. A typical computed tomography scan finding of an appendiceal mucocele is a round, low-density, thin-walled, encapsulated mass, communicating with the cecum. Ultrasonography shows a cystic, encapsulated lesion, firmly attached to the cecum, with liquid content and an internal variable echogenicity related to mucus density. Colonoscopy may show a pathogn-omonic image, the ‘sign of the volcano’ , i.e., an erythematous, soft mass with a central crater, from which mucus is discharged[12-15].
Therapy is surgical, but laparoscopic approach is not advised because of the risk of rupture[16].
The type of surgical treatment is related to the dimensions and to histology of the mucocele. Appendectomy is used for simple mucocele or for cystoadenoma, when the appendiceal base is intact. Cecal resection is indicated for cystoadenoma with a large base, and a right hemi-colectomy is recommended for cystoadenocarcinoma. Intra-operative histologic examination is not always definitive. An accurate exploration of the abdomen during laparotomy is advised, because of the association between the appendiceal mucocele and other tumors, particularly carcinoma of the colon (11-20 %) and tumors of the ovary[17].
If exploration reveals a ruptured appendiceal mucocele, the primary resection should be accompanied by removal of all gross implants [16,17].
Postoperatively, patients with simple or benign neoplastic mucoceles have shown an excellent prognosis with 5-year survival rates of 91-100%, even in cases with extension of mucus into the extra-appendiceal spaces. In malignant mucoceles, however, the 5-year survival rate is markedly diminished (25%) due to complications of pseudomyxoma peritonei[1].
In conclusion, patients with mucoceles can present with various symptoms, but may also be asymptomatic. Preope-rative diagnosis is rare, but it is possible using appropriate tests. These uncommon and potentially lethal entities are usually surgically curable, if diagnosed in an early phase. Therefore, pre-operative recognition with a carefully planned resection to remove the mass is required.
Science Editor Li WZ Language Editor Elsevier HK
| 1. | Aho AJ, Heinonen R, Laurén P. Benign and malignant mucocele of the appendix. Histological types and prognosis. Acta Chir Scand. 1973;139:392-400. [PubMed] [Cited in This Article: ] |
| 2. | Crawford J; Tumors of the appendix. In: Cotran R, Kumar V, Robbins S, eds. Pathologic basis of disease. Philadelphia Saunders 1994, 824-825. . [Cited in This Article: ] |
| 3. | Landen S, Bertrand C, Maddern GJ, Herman D, Pourbaix A, de Neve A, Schmitz A. Appendiceal mucoceles and pseudomyxoma peritonei. Surg Gynecol Obstet. 1992;175:401-404. [PubMed] [Cited in This Article: ] |
| 4. | Higa E, Rosai J, Pizzimbono CA, Wise L. Mucosal hyperplasia, mucinous cystadenoma, and mucinous cystadenocarcinoma of the appendix. A re-evaluation of appendiceal "mucocele". Cancer. 1973;32:1525-1541. [PubMed] [DOI] [Cited in This Article: ] [Cited by in F6Publishing: 2] [Reference Citation Analysis (0)] |
| 5. | Gibbs NM. Mucinous cystadenoma and cystadenocarcinoma of the vermiform appendix with particular reference to mucocele and pseudomyxoma peritonei. J Clin Pathol. 1973;26:413-421. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 64] [Cited by in F6Publishing: 69] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 6. | Merran S. [Mucus secreting tumor of the appendix (appendiceal mucocele)]. Presse Med. 1997;26:933. [PubMed] [Cited in This Article: ] |
| 7. | Peek DF, Beets GL. Pseudomyxoma peritonei in the pleural cavity: report of a case. Dis Colon Rectum. 1999;42:113-15; discussion 113-15;. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 13] [Cited by in F6Publishing: 15] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 8. | Takahashi S, Furukawa T, Ueda J. Case report: Mucocele of the tip of the appendix. Clin Radiol. 1998;53:149-150. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 16] [Cited by in F6Publishing: 16] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 9. | Stevens KJ, Dunn WK, Balfour T. Pseudomyxoma extraperitonei: a lethal complication of mucinous adenocarcinoma of the appendix. Am J Gastroenterol. 1997;92:1920-1922. [PubMed] [Cited in This Article: ] |
| 10. | Dachman AH, Lichtenstein JE, Friedman AC. Mucocele of the appendix and pseudomyxoma peritonei. AJR Am J Roentgenol. 1985;144:923-929. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 103] [Cited by in F6Publishing: 108] [Article Influence: 2.8] [Reference Citation Analysis (0)] |
| 11. | Soweid AM, Clarkston WK, Andrus CH, Janney CG. Diagnosis and management of appendiceal mucoceles. Dig Dis. 1998;16:183-186. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 44] [Cited by in F6Publishing: 49] [Article Influence: 1.9] [Reference Citation Analysis (0)] |
| 12. | Kim SH, Lim HK, Lee WJ, Lim JH, Byun JY. Mucocele of the appendix: ultrasonographic and CT findings. Abdom Imaging. 1998;23:292-296. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 88] [Cited by in F6Publishing: 75] [Article Influence: 2.9] [Reference Citation Analysis (0)] |
| 13. | Zissin R, Gayer G, Kots E, Apter S, Peri M, Shapiro-Feinberg M. Imaging of mucocoele of the appendix with emphasis on the CT findings: a report of 10 cases. Clin Radiol. 1999;54:826-832. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 49] [Cited by in F6Publishing: 53] [Article Influence: 2.1] [Reference Citation Analysis (0)] |
| 14. | Isaacs KL, Warshauer DM. Mucocele of the appendix: computed tomographic, endoscopic, and pathologic correlation. Am J Gastroenterol. 1992;87:787-789. [PubMed] [Cited in This Article: ] |
| 15. | Hamilton DL, Stormont JM. The volcano sign of appendiceal mucocele. Gastrointest Endosc. 1989;35:453-456. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 40] [Cited by in F6Publishing: 43] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 16. | González Moreno S, Shmookler BM, Sugarbaker PH. Appendiceal mucocele. Contraindication to laparoscopic appendectomy. Surg Endosc. 1998;12:1177-1179. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 86] [Cited by in F6Publishing: 94] [Article Influence: 3.6] [Reference Citation Analysis (0)] |
| 17. | Kahn M, Friedman IH. Mucocele of the appendix: diagnosis and surgical management. Dis Colon Rectum. 1979;22:267-269. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 32] [Cited by in F6Publishing: 31] [Article Influence: 0.7] [Reference Citation Analysis (0)] |