Copyright
©The Author(s) 2021.
World J Gastroenterol. Dec 14, 2021; 27(46): 8010-8030
Published online Dec 14, 2021. doi: 10.3748/wjg.v27.i46.8010
Published online Dec 14, 2021. doi: 10.3748/wjg.v27.i46.8010
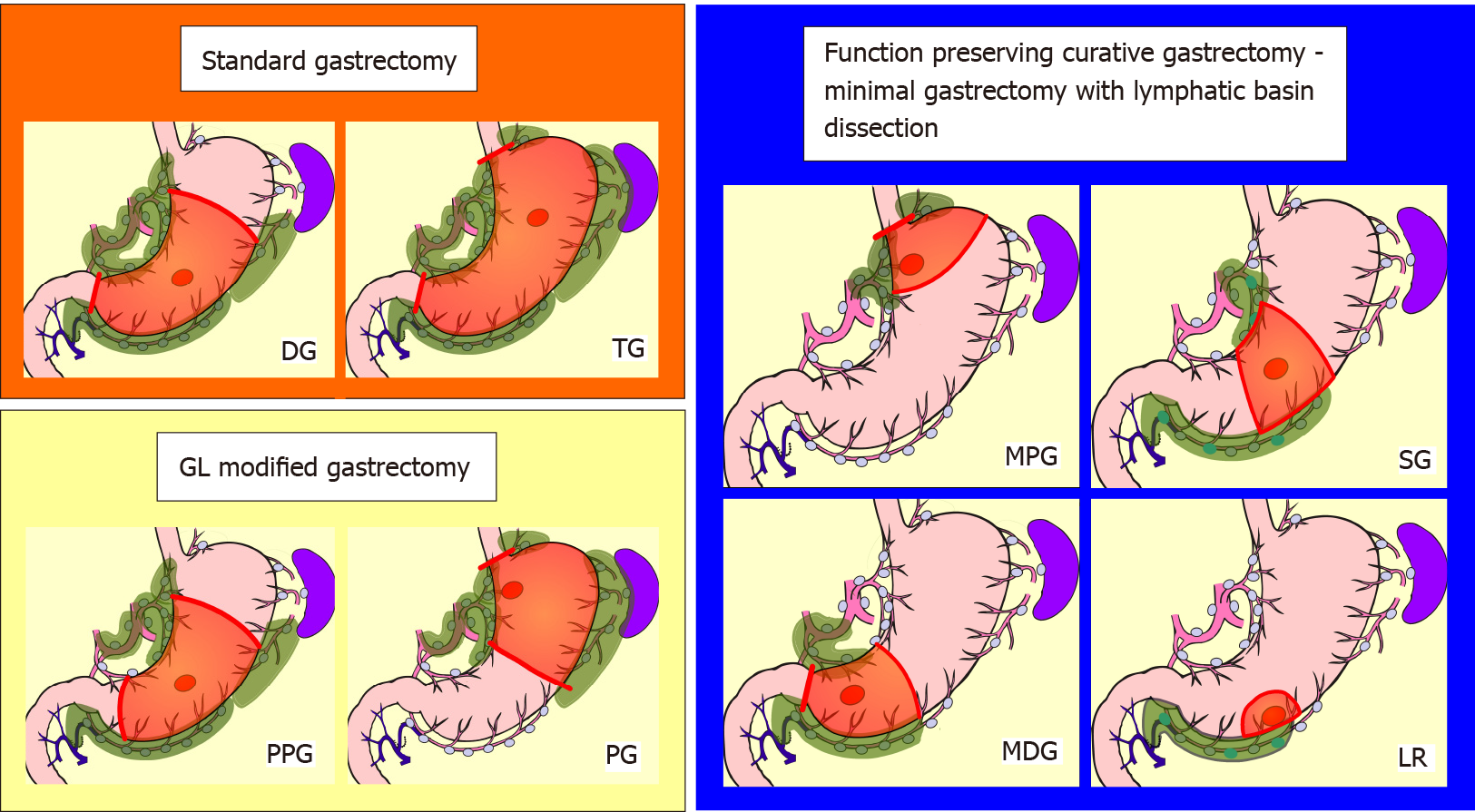
Figure 1 Schemas of standard gastrectomy, modified gastrectomy due to guidelines, and the function-preserving curative gastrectomy with lymphatic basin dissection.
The red circle indicates the tumor, the green colored area indicates the extent of lymph node dissection, and the orange area indicates the extent of gastrectomy. The extent of nodal dissection in standard gastrectomy and modified gastrectomy according to the guidelines was D1 +. In contrast, the extent of nodal dissection in lymphatic basin dissection was defined as D0. GL: Japanese gastric cancer treatment guidelines; DG: Distal gastrectomy; TG: Total gastrectomy; PPG: Pylorus-preserving gastrectomy; PG: Proximal gastrectomy; MPG: Mini-proximal gastrectomy; SG: Segmental gastrectomy; MDG: Mini-distal gastrectomy; LR: Local resection.
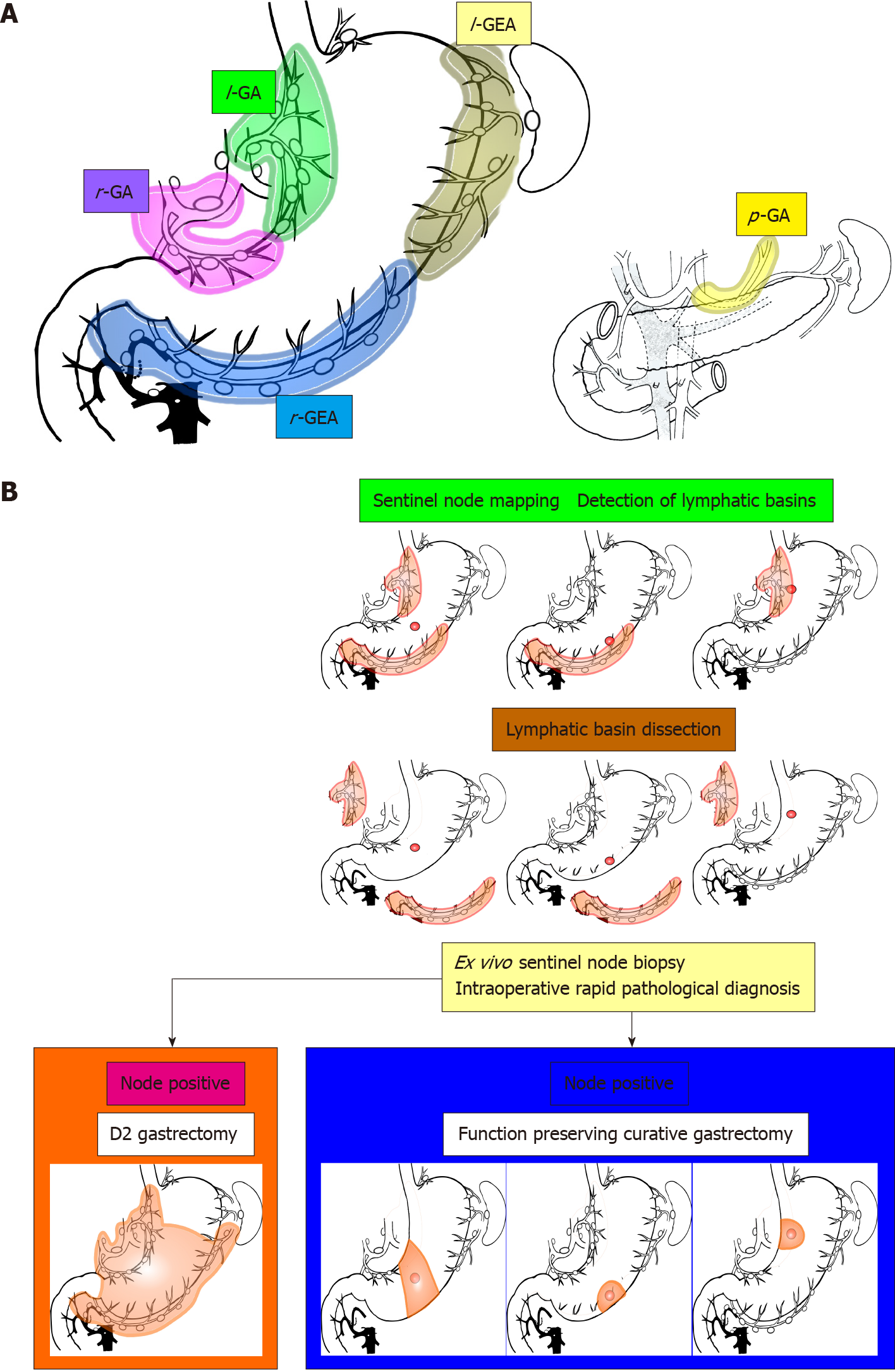
Figure 2 Lymphatic basins, lymphatic compartments, and the strategy of sentinel node navigation surgery.
A: The lymphatic basins were defined as the lymphatic system that was detected with dyed or fluorescent lymphatics. The lymphatic basins were integrated into the five lymphatic areas. Each of these was called the lymphatic compartment and was classified into five basins; B: Algorithm for sentinel node navigation surgery for early gastric cancer. First, sentinel node mapping was performed, followed by lymphatic basin dissection, ex vivo identification and biopsy of the sentinel nodes, and intraoperative rapid pathology. If the sentinel nodes were diagnosed as metastasis at rapid diagnosis, standard gastrectomy with nodal dissection up to D2 was performed; if the sentinel nodes were diagnosed as node negative, the extent of gastrectomy was reduced and function-preserving curative gastrectomy, such as segmental gastrectomy or local resection, was applied. l-GA: Left gastric artery basin; r-GA: Right gastric artery basin; l-GEA: Left gastroepiploic artery basin; r-GEA: Right gastroepiploic artery basin; p-GA: Posterior gastric artery basin.
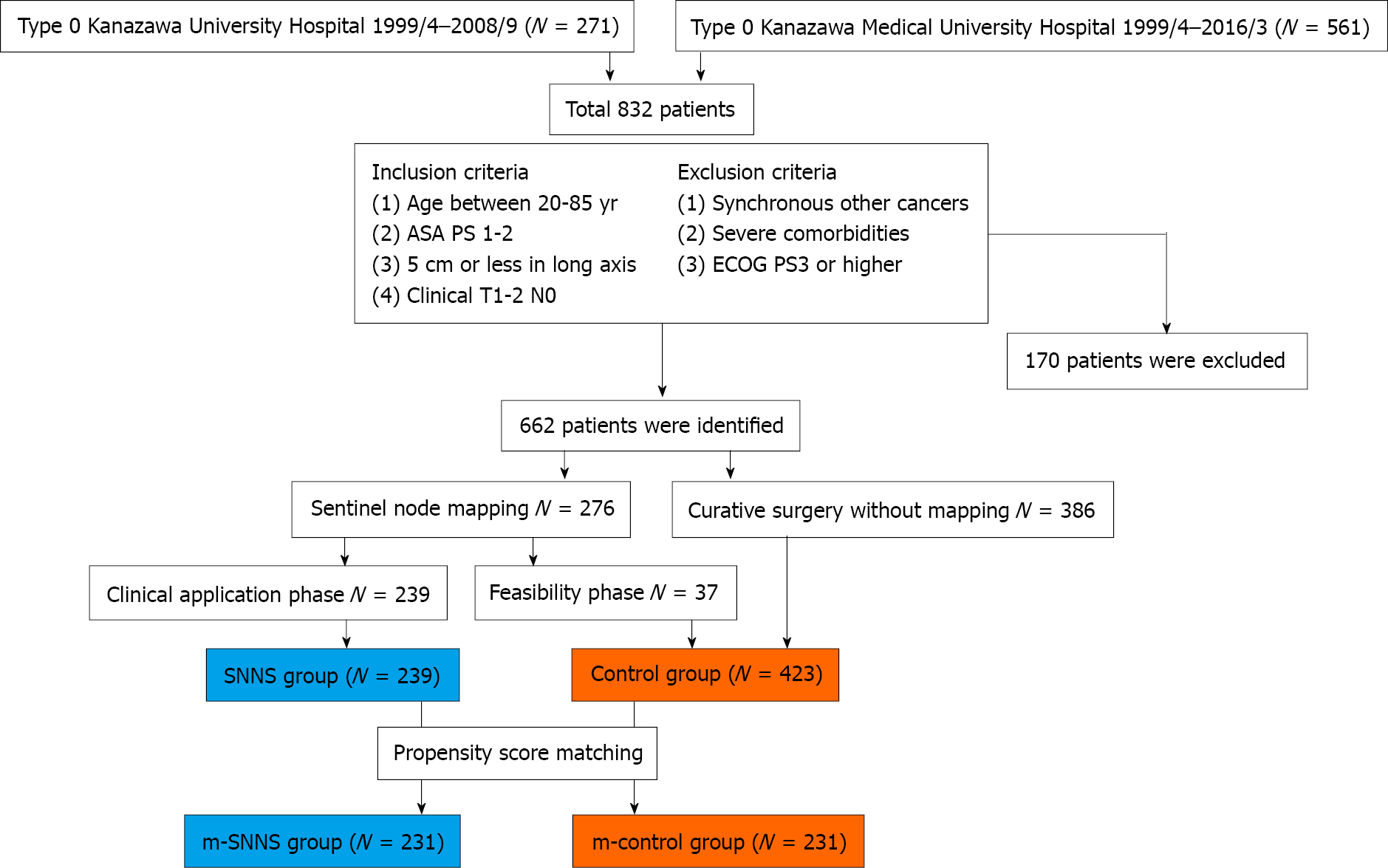
Figure 3 Summary of enrolled patients.
The control group consisted of patients who underwent guidelines gastrectomy with standard lymph node dissection, while the sentinel node navigation surgery (SNNS) group consisted of patients who underwent tailor-made gastrectomy guided by sentinel node biopsy. SNNS: Sentinel node navigation surgery; m-SNNS: Propensity score-matched sentinel node navigation surgery; m-control: Propensity score-matched control; ECOG: Eastern Cooperative Oncology Group; ASA PS: American Society of Anesthesiologists physical status.
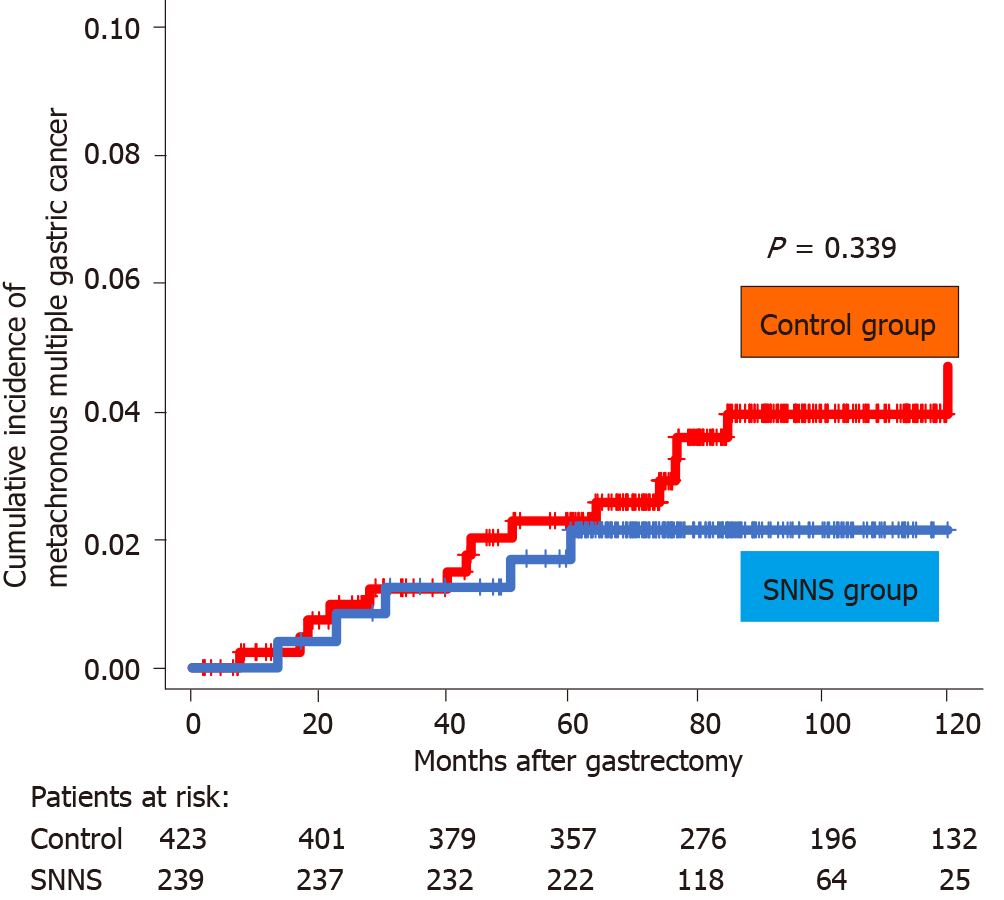
Figure 4 Cumulative incidence of metachronous multiple gastric cancer in the remnant stomach.
There was no difference in the incidence of metachronous multiple gastric cancer between the SNNS and control groups. SNNS: sentinel node navigation surgery.
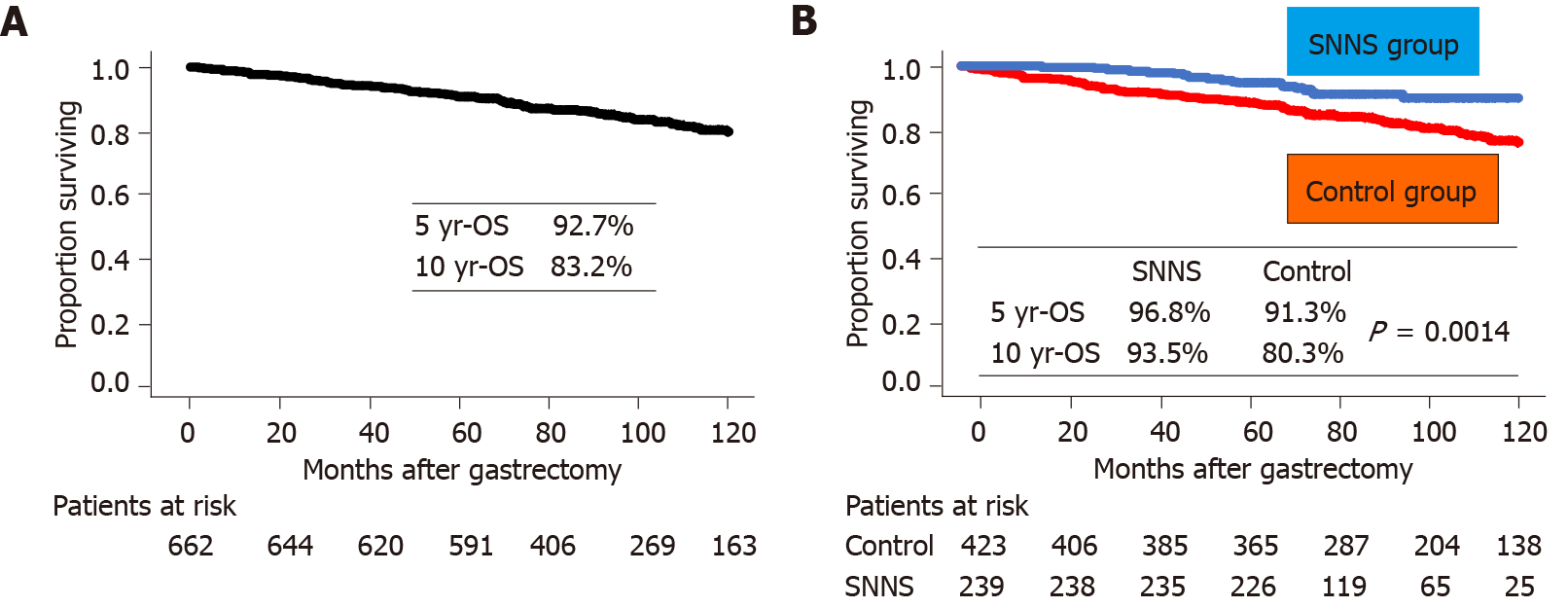
Figure 5 Overall survival curve.
A: The overall survival of all patients; B: Comparison of overall survival between the sentinel node navigation surgery (SNNS) and control groups. The overall survival of the SNNS group was significantly better than the control group. SNNS: Sentinel node navigation surgery; OS: Overall survival.
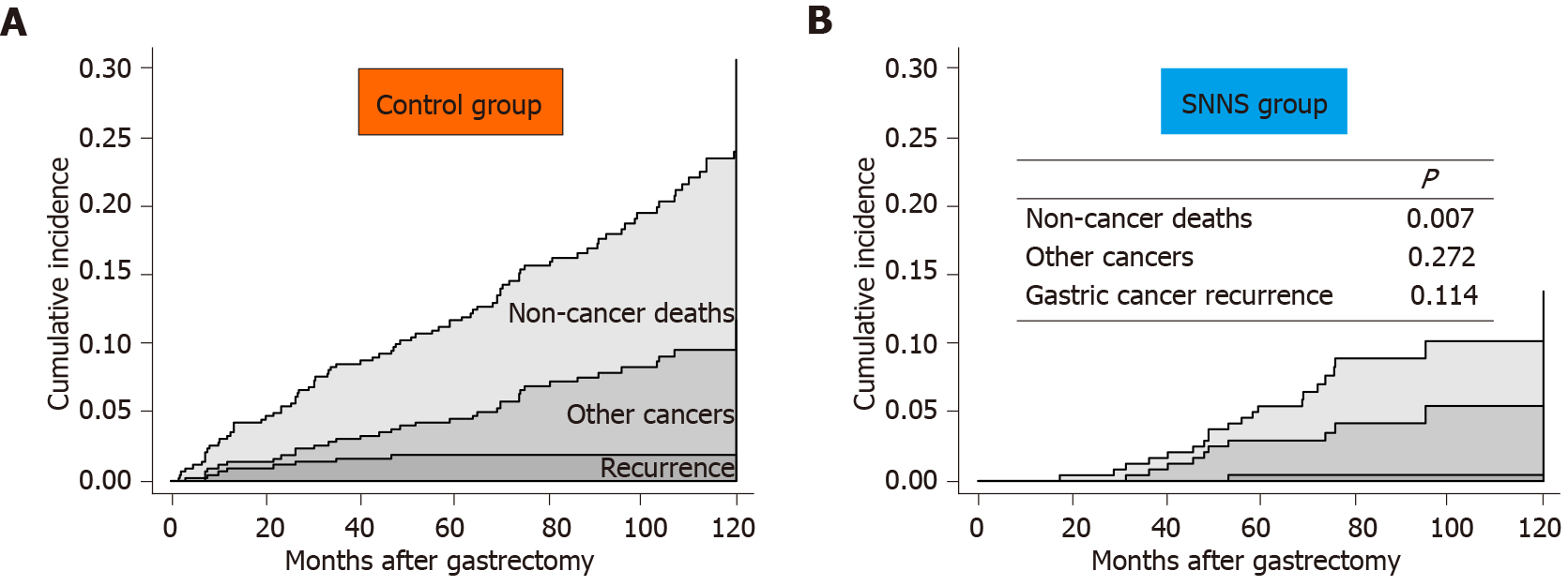
Figure 6 Cumulative incidence of gastric cancer recurrence or reason for death.
A: Control group; B: Sentinel node navigation surgery (SNNS) group. The cumulative incidence of gastric cancer recurrence and other cancer-related deaths was almost equal between the two groups; in contrast, that of non-cancer deaths from other diseases was lower in the SNNS group than in the control group. SNNS: Sentinel node navigation surgery.
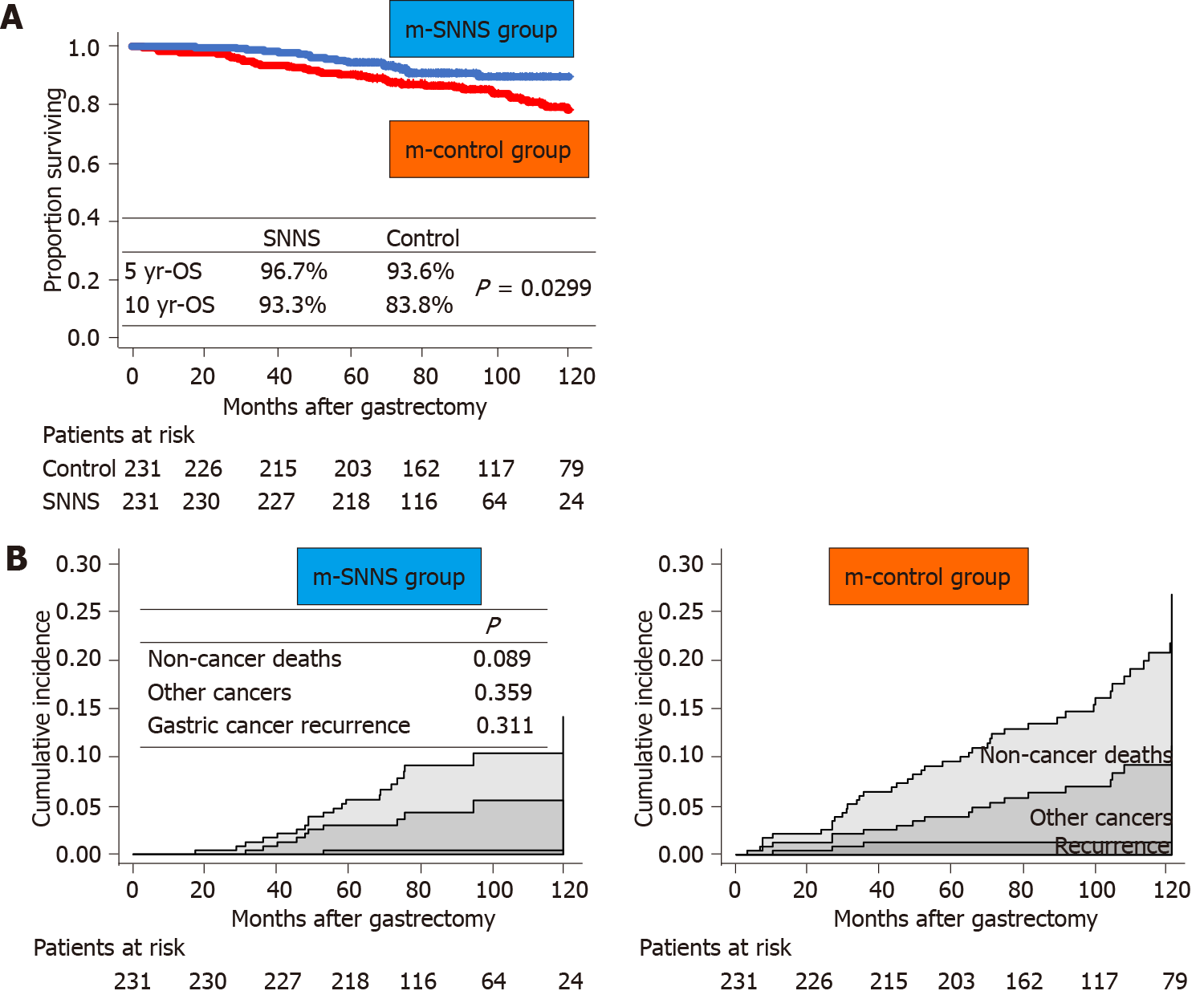
Figure 7 Comparisons of overall survival and cumulative incidence between the two groups after propensity score matching.
A: Overall survival curves; B: Cumulative incidence curves of gastric cancer recurrence or the reason for death. The overall survival of the sentinel node navigation surgery (SNNS) group was significantly better than that of the control group. The cumulative recurrence of non-cancer deaths from other diseases in the SNNS group tended to be lower than that in the control group. SNNS: Sentinel node navigation surgery; m-SNNS: Propensity score-matched sentinel node navigation surgery; m-control: Propensity score-matched control; OS: Overall survival.
- Citation: Kinami S, Nakamura N, Miyashita T, Kitakata H, Fushida S, Fujimura T, Iida Y, Inaki N, Ito T, Takamura H. Life prognosis of sentinel node navigation surgery for early-stage gastric cancer: Outcome of lymphatic basin dissection. World J Gastroenterol 2021; 27(46): 8010-8030
- URL: https://www.wjgnet.com/1007-9327/full/v27/i46/8010.htm
- DOI: https://dx.doi.org/10.3748/wjg.v27.i46.8010