Copyright
©2014 Baishideng Publishing Group Inc.
World J Gastroenterol. Aug 28, 2014; 20(32): 11080-11094
Published online Aug 28, 2014. doi: 10.3748/wjg.v20.i32.11080
Published online Aug 28, 2014. doi: 10.3748/wjg.v20.i32.11080
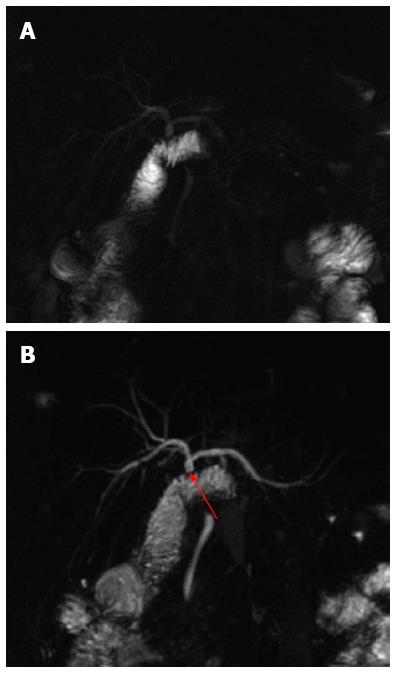
Figure 1 Bilio-enteric anastomosis.
A: Single-shot thick-slab magnetic resonance cholangiogram shows a regular hepatico-jejunostomy; B: Maximum intensity projection reconstruction of 3D thin-slab fast spin-echo T2-weighted images confirms the anastomotic patency (red arrow) and better demonstrates the portion of the jejunum and the choledocho of the recipient.
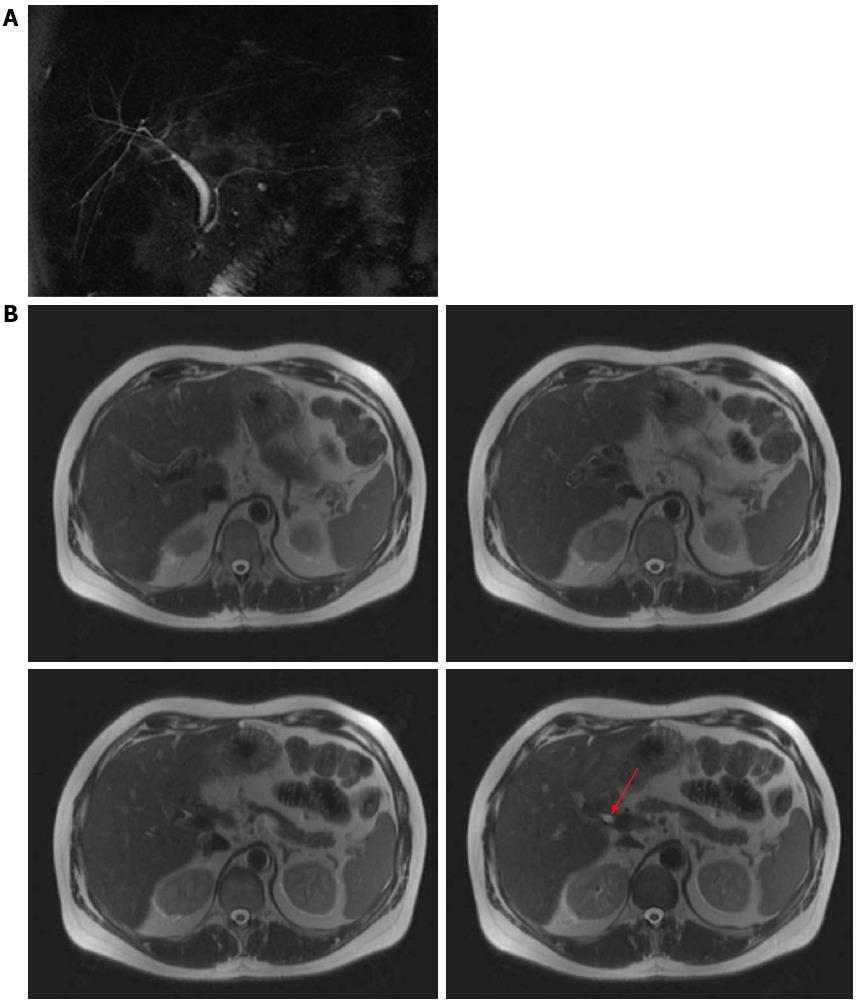
Figure 2 Duct-to-duct anastomosis.
A: Single-shot thick-slab magnetic resonance cholangiogram shows a choledocho-choledocho anastomosis with a discrepancy of caliber between donor and recipient choledocho; B: Axial single-shot T2-weighted images demonstrate the anastomotic patency (red arrow).
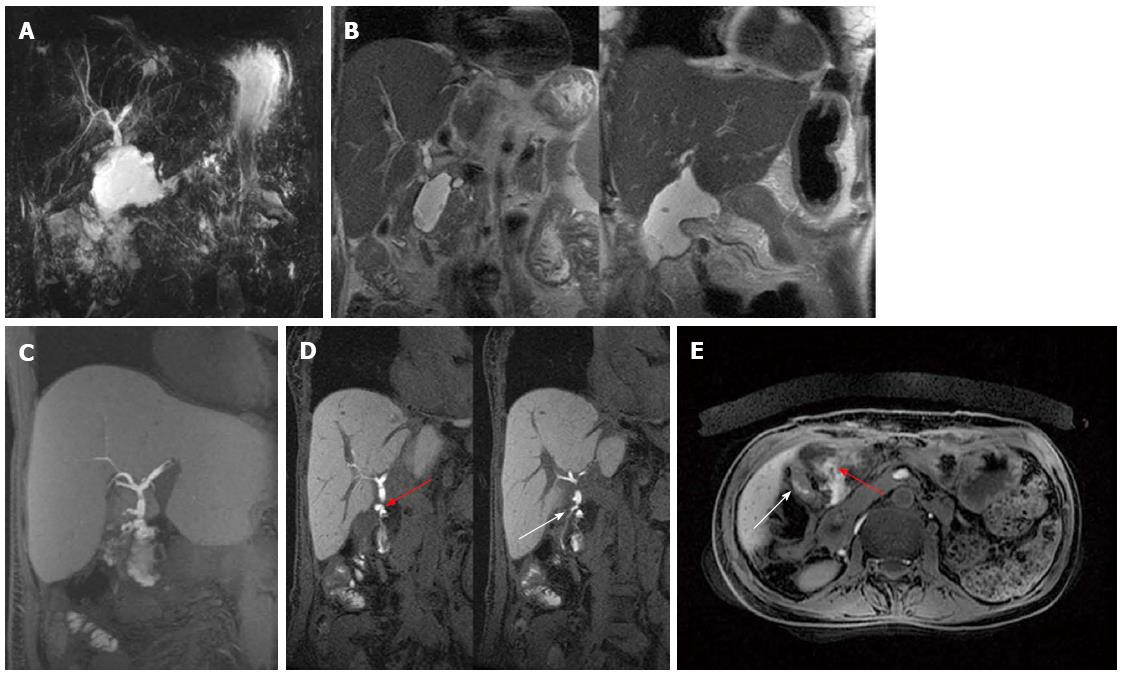
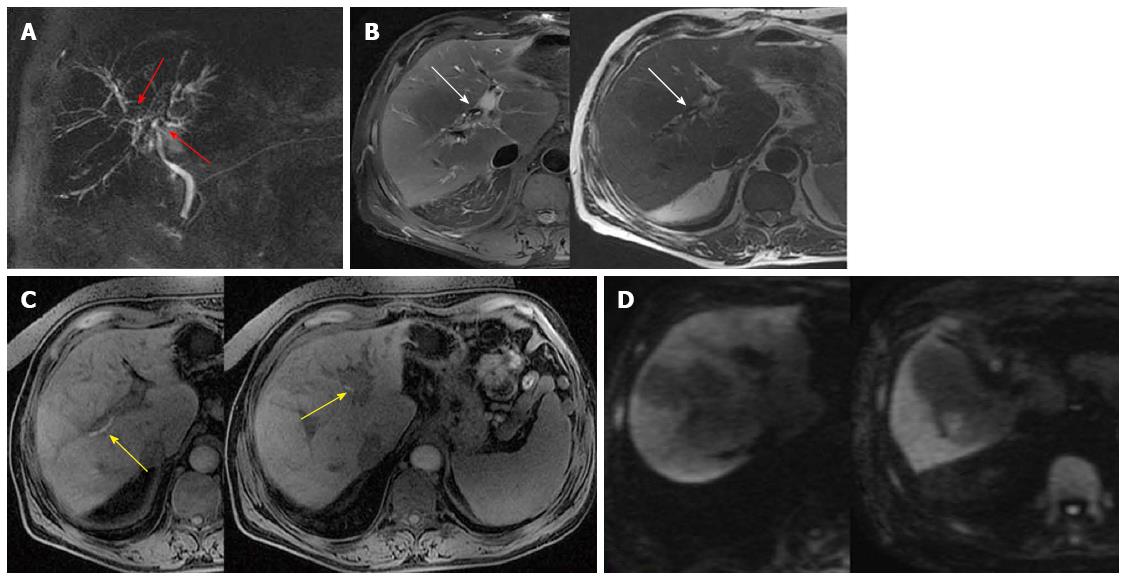
Figure 3 Anastomotic leak in a patient with hepatico-jejunostomy.
A: Single-shot thick-slab magnetic resonance cholangiogram shows a fluid collection in the area of biliary-enteric anastomosis; B: Coronal T2-weighted images (at different levels) accurately depict circumscribed sub-hepatic fluid collections with thickened walls. C: Maximum intensity projection reconstruction of Gd-EOB-DTPA enhanced LAVA T1-weighted sequence well exhibits extravasation of contrast material into the peri-anastomotic space compatible with bile leak; D: Coronal Gd-EOB-DTPA enhanced LAVA T1-weighted images better identify contrast agent both extravasating from an anastomotic leak (red arrow) and filling the Roux-en-Y anastomosis (white arrow); E: On axial post-contrast LAVA image it is possible to distinguish the fluid collection (red arrow) from the jejunum (white arrow).
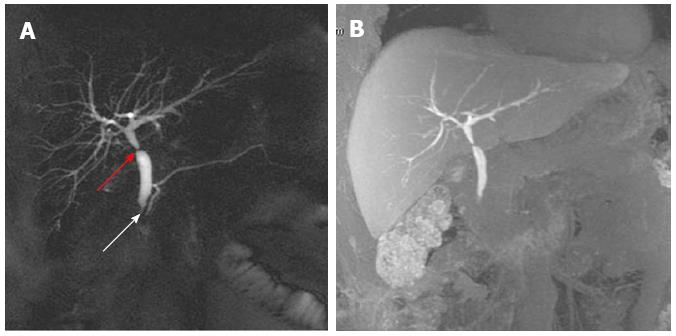
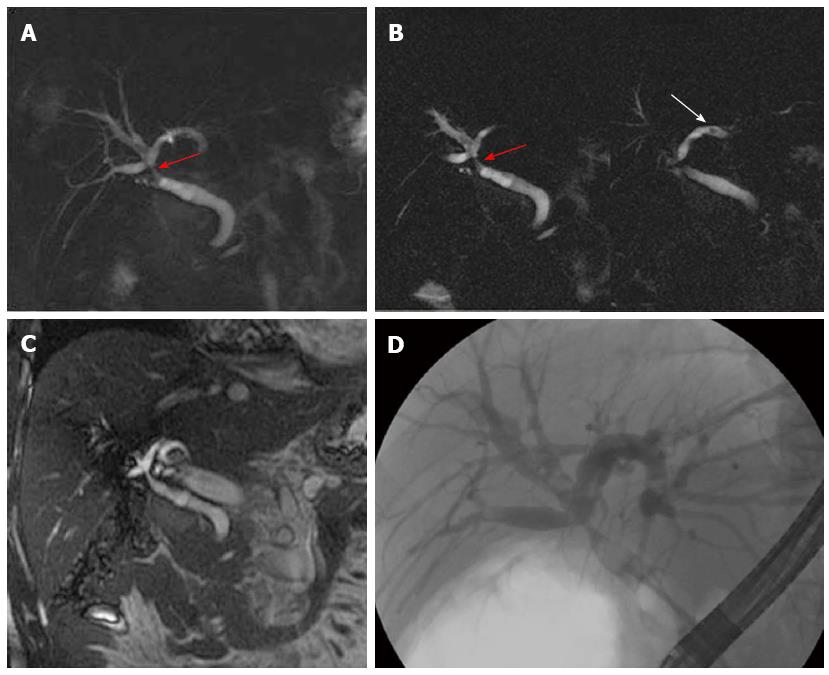
Figure 4 Anastomotic biliary stricture associated with sphincter of Oddi dysfunction.
A: Single-shot thick-slab magnetic resonance cholangiogram shows stricture of both anastomotic site (red arrow) and iuxta-papillary choledocho (white arrow), with dilation of pre- and post-anastomotic biliary tract; B: Maximum intensity projection reconstruction of Gd-EOB-DTPA enhanced T1-weighted LAVA sequence demonstrates regular excretion of contrast-enhanced bile in the extra-hepatic biliary tract at 20 min, while contrast-enhanced bile excretion in the duodenum is not appreciable.
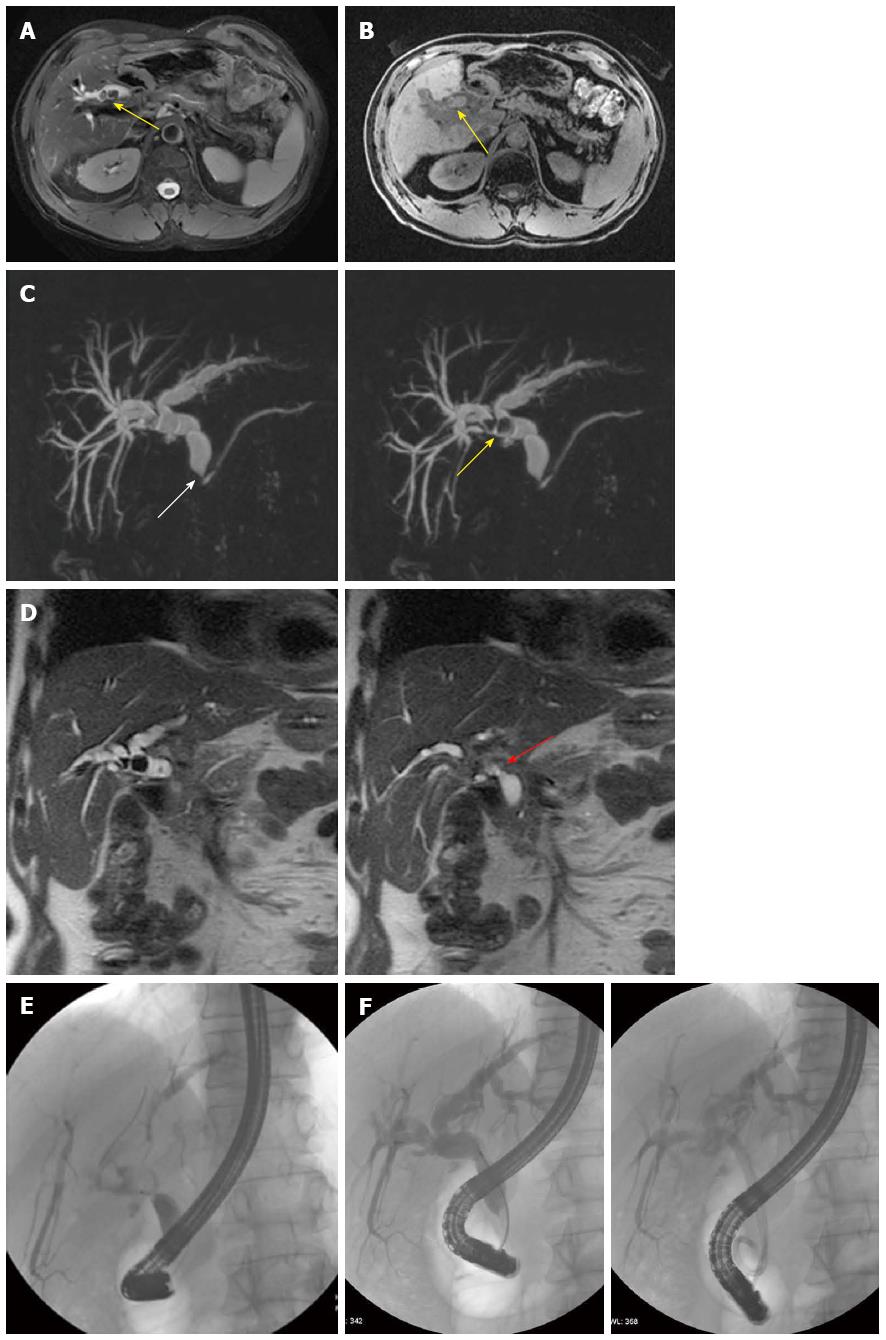
Figure 5 Anastomotic biliary stricture with lithiasis.
A: Axial T2-weighted image shows dilation of the biliary system with concomitant stones (yellow arrow); B: Axial T1-weighted image confirms the presence of stones in the biliary tract (yellow arrow); C: Maximum intensity projections of 3D thin-slab fast spin-echo T2-weighted images (obtained using different thicknesses) demonstrate the dilation of the both intra- and extra-hepatic (pre- and post-anastomotic) biliary tract with a stricture of the iuxta-papillary choledocho (white arrow); the presence of two stones at the level of the hepatic bifurcation (yellow arrow) is also well appreciable; D: On coronal single-shot T2-weighted images (at different levels) is also better appreciable a stricture at the anastomotic site (red arrow); E: Endoscopic retrograde cholangiography confirms the presence of strictures and stones in the pre-anastomotic biliary tract; F: Stones were endoscopically removed and strictures were treated by stenting as shown on different projection images.
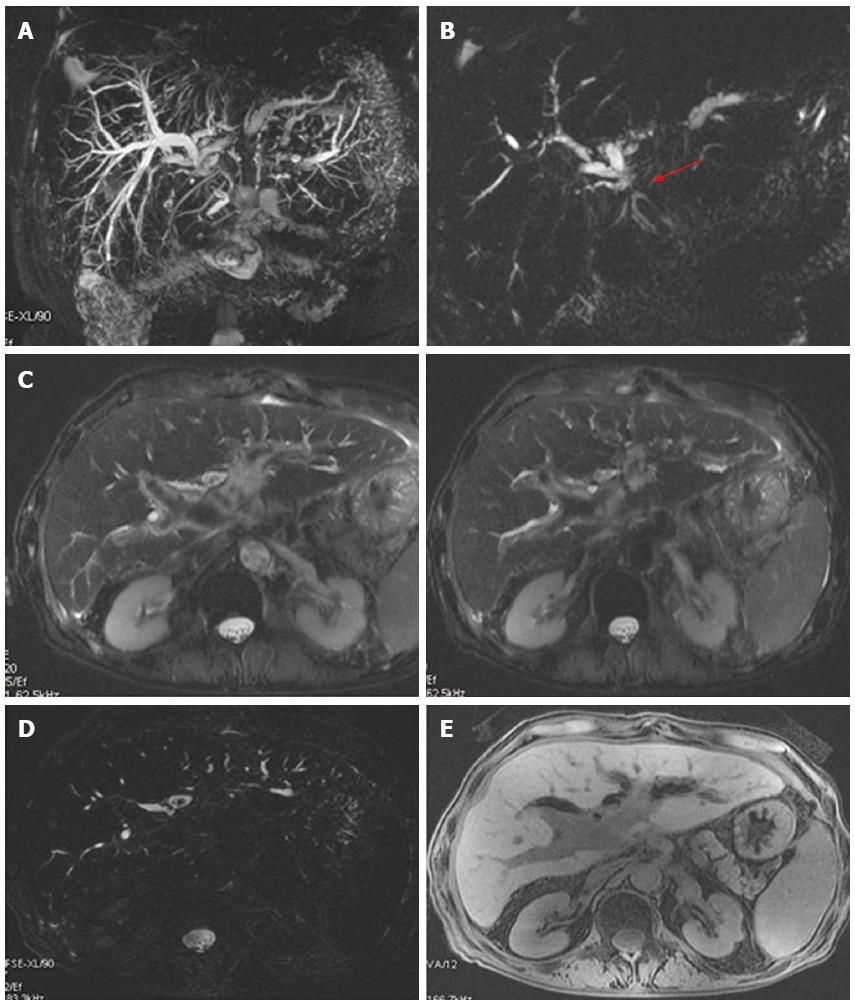
Figure 6 Anastomotic biliary stricture with lithiasis in a patient with hepatico-jejunostomy.
A: Maximum intensity projection reconstruction of 3D thin-slab fast spin-echo T2-weighted images shows marked dilation of the biliary system with partial visualization of the left hepatic duct; B: Single-shot thick-slab magnetic resonance cholangiogram well depicts the stricture of the anastomotic site (red arrow); C, D: Axial single-shot T2-weighted images and axial 3D thin-slab fast spin-echo T2-weighted image demonstrate dilation of the pre-anastomotic biliary tract with the presence of pneumobilia, in particular at the level of left and common hepatic ducts with concomitant stones into the left one; E: Axial T1-weighted image better recognizes pneumobilia.
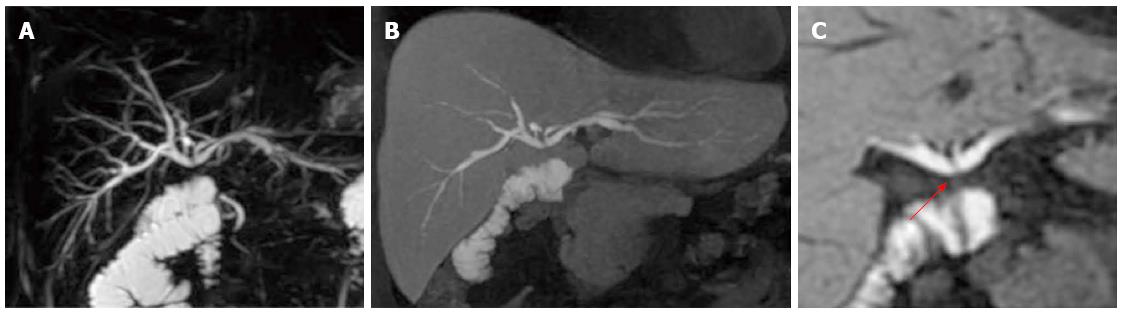
Figure 7 Patent anastomosis in a patient with hepatico-jejunostomy.
A: Coronal T2-weighted magnetic resonance cholangiography reveals a moderate dilation of the intrahepatic biliary system, but does not visualize the site of the biliary-enteric anastomosis; B, C: Coronal Gd-EOB-DTPA-enhanced T1-weighted magnetic resonance cholangiogram, obtained 20 min after contrast injection, shows contrast excretion into the intrahepatic biliary system, the site of biliary-enteric anastomosis (red arrow) and anastomotic jejunal loop, demonstrating the patency of the biliary-enteric anastomosis.
Figure 8 Non-anastomotic biliary stricture: Early ischemic type biliary lesion.
A: Single-shot thick-slab magnetic resonance cholangiogram demonstrates discrepancy of caliber between donor and recipient extrahepatic biliary tract without dilation of intrahepatic biliary system; B: T-tube cholangiography confirms the presence of the mild stenosis; C: Axial T2-weighted images well exhibit the presence of circumferential wall thickening of the extrahepatic biliary tree of the graft (red arrows).
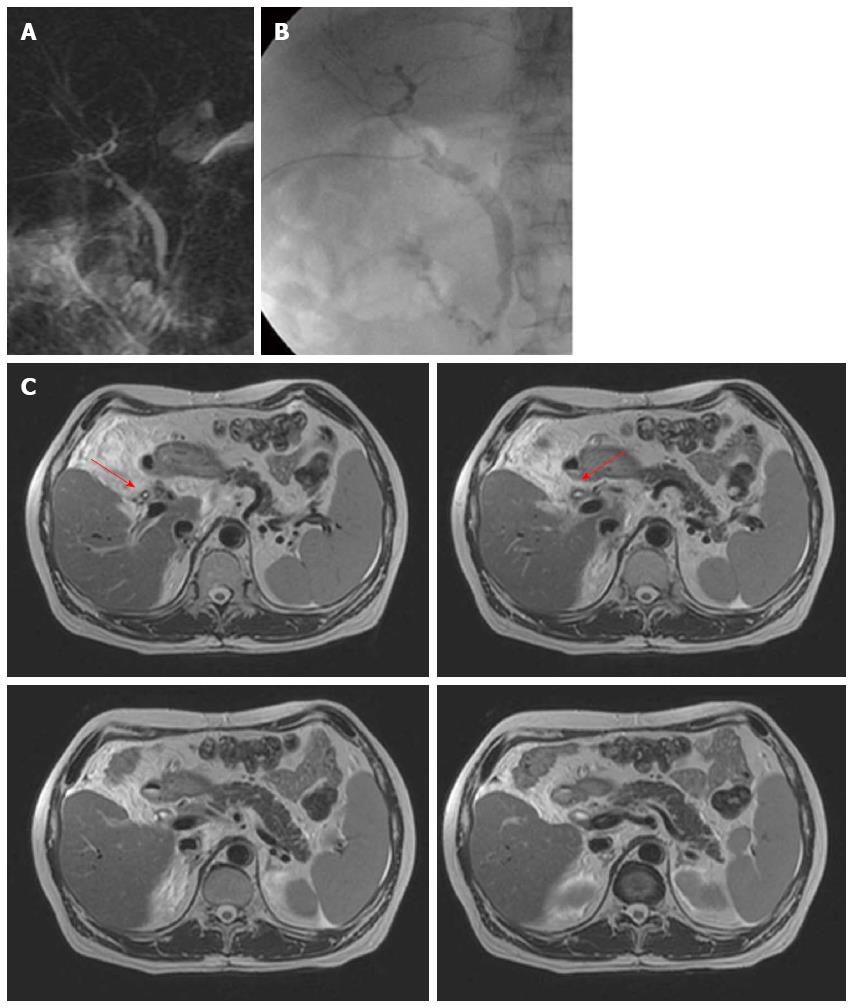
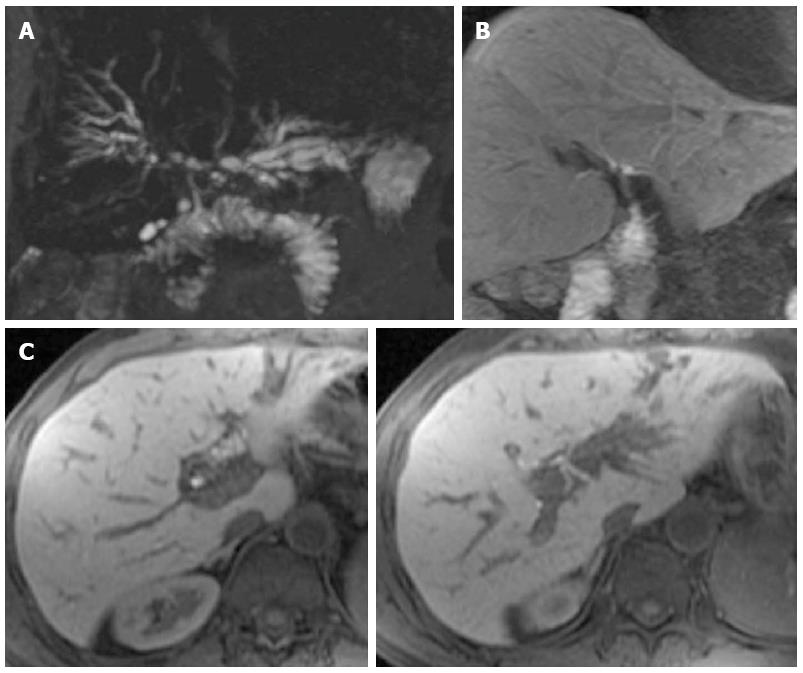
Figure 9 Non-anastomotic biliary stricture: Advanced ischemic type biliary lesion.
A: Single-shot thick-slab magnetic resonance cholangiogram demonstrates a stenosis of the hepatic bifurcation and hepatic ducts (red arrows) with an irregular dilation of the intrahepatic biliary system; B, C: Axial T2- and axial T1-weighted images well exhibit the presence of circumferential wall thickening (white arrows) at the level of hepatic bifurcation and endoluminal casts (yellow arrows); D: On diffusion-weighted imaging the liver parenchyma appears inhomogeneous with multiples areas of persistent high signal intensity in highest b-value acquisitions.
Figure 10 Non-anastomotic biliary stricture: Classic signs of ischemic type biliary lesion.
A, B: Single-shot thick-slab magnetic resonance cholangiopancreatography show the stricture at the level of hepatic bifurcation (red arrow) and the presence of biliary sludge/stones (white arrow) in the dilated intrahepatic biliary system; C: On coronal T2-weighted image the wall thickening of the extrahepatic biliary tree of the graft is also well appreciable; D: Endoscopic retrograde cholangiography exhibits the optimal correlation of these features.
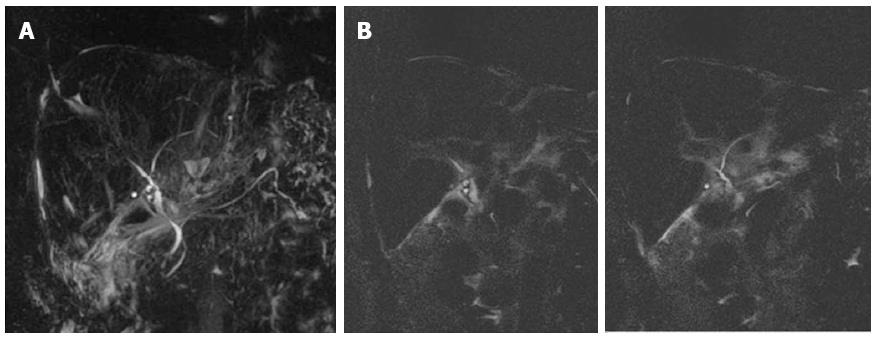
Figure 11 Recurrence of primary sclerosing cholangitis in a transplant patient with hepatico-jejunostomy.
A: Maximum intensity projection (MIP) reconstruction of 3D thin-slab fast spin-echo T2-weighted images shows multifocal stenosis with intervening saccular dilation affecting the intrahepatic biliary system; B, C: On MIP reconstruction and axial Gd-EOB-DTPA enhanced LAVA T1-weighted sequences the intrahepatic biliary system is not appreciable, however the irregularities of the extrahepatic biliary tract are more accurately depicted.
Figure 12 Vanishing bile duct syndrome.
A: Maximum intensity projection reconstruction of 3D thin-slab fast spin-echo T2-weighted images shows only extrahepatic pre- and post-anastomotic biliary tract; the entire intrahepatic biliary system is missed; B: These findings are better appreciable on single-shot thin-slab magnetic resonance cholangiograms.
- Citation: Boraschi P, Donati F. Postoperative biliary adverse events following orthotopic liver transplantation: Assessment with magnetic resonance cholangiography. World J Gastroenterol 2014; 20(32): 11080-11094
- URL: https://www.wjgnet.com/1007-9327/full/v20/i32/11080.htm
- DOI: https://dx.doi.org/10.3748/wjg.v20.i32.11080