Copyright
©2014 Baishideng Publishing Group Co.
World J Gastroenterol. Apr 7, 2014; 20(13): 3443-3456
Published online Apr 7, 2014. doi: 10.3748/wjg.v20.i13.3443
Published online Apr 7, 2014. doi: 10.3748/wjg.v20.i13.3443
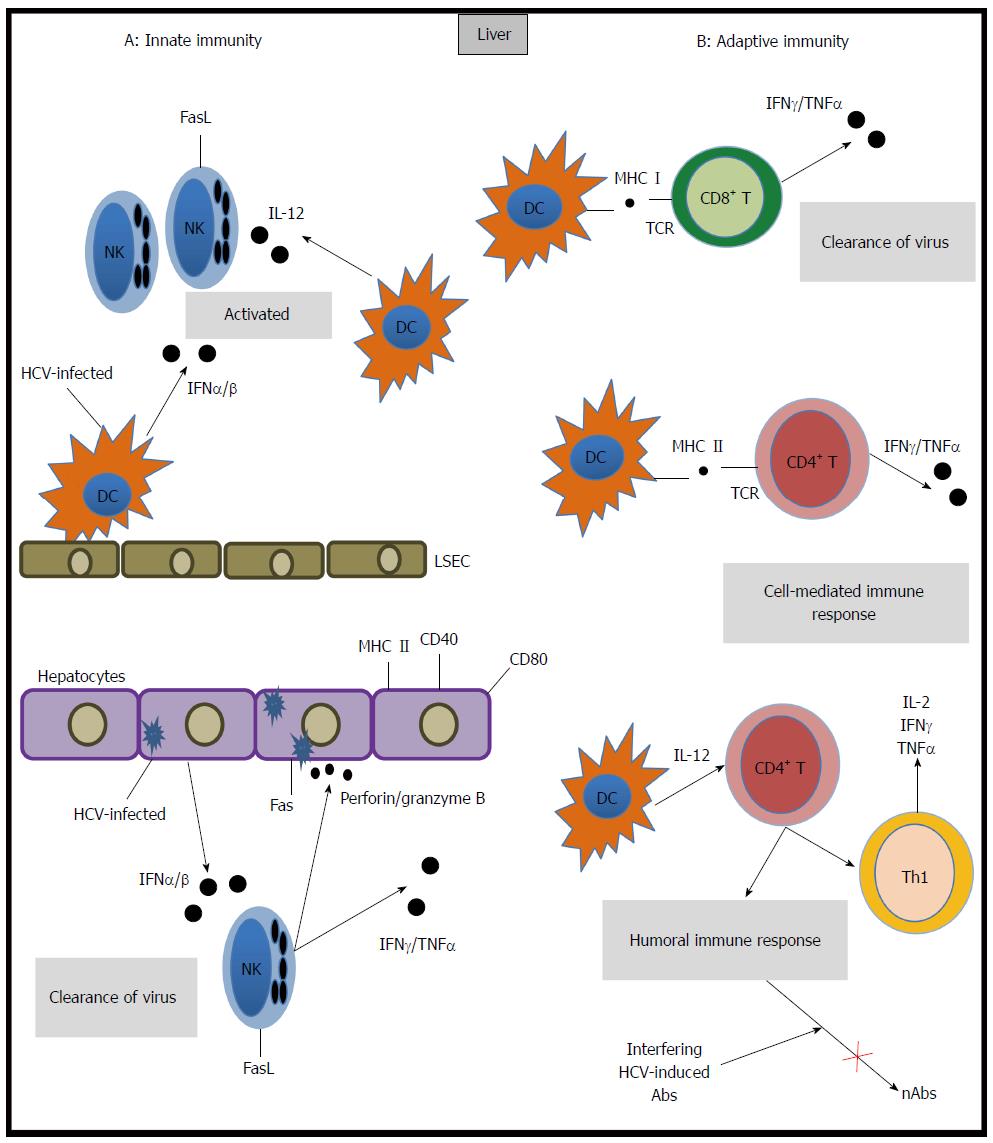
Figure 1 Mechanisms of Immune response to hepatitis C virus.
Multiple innate (A) and adaptive immune (B) components are involved in hepatitis C virus (HCV) infection (see text), dendritic cells (DC), natural killer (NK) cells, CD4+, CD8+ T cells and B-cell mediated humoral immune response are crucial for disease outcome. IFN-γ: interferon-gamma; TNF-α: tumor necrosis factor-α; IL: Interleukin; nAbs: Neutralizing anti-HCV antibodies.
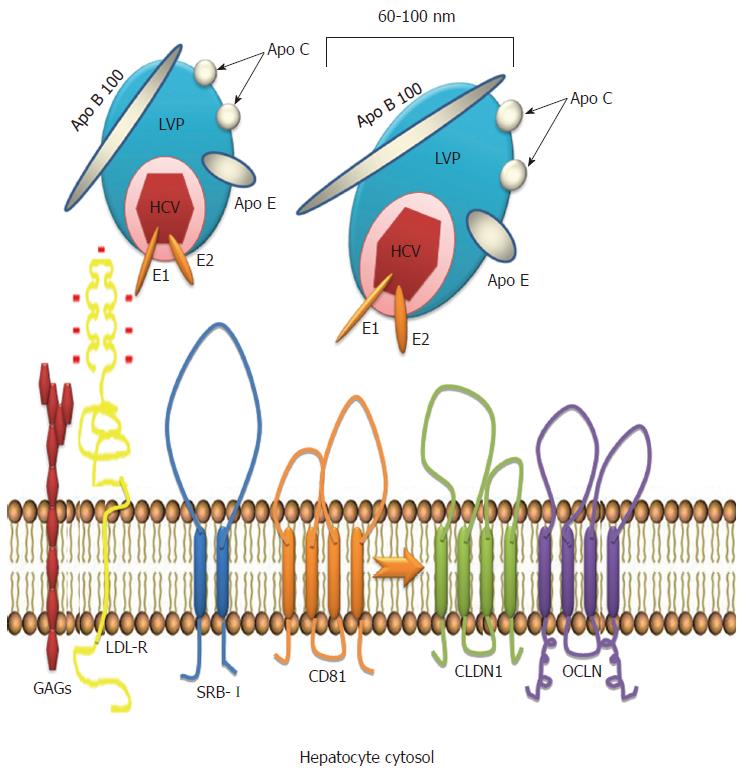
Figure 2 Hepatitis C virus entry.
Hepatitis C virus (HCV) binds to lipoproteins and forms the lipo viro particle (LVP). LVP is attached by the hepatic low density lipoprotein (LDL) receptors through viral surface membrane proteins E1 and E2. After the initial phase, the LVP interacts with several input factors: the scavenger receptor class B type I (SRB-I), the membrane receptor CD81, coreceptors claudin 1 (CLDN1) and ocludin (OCLN). LVP is internalized into the cytosol by endocytosis.
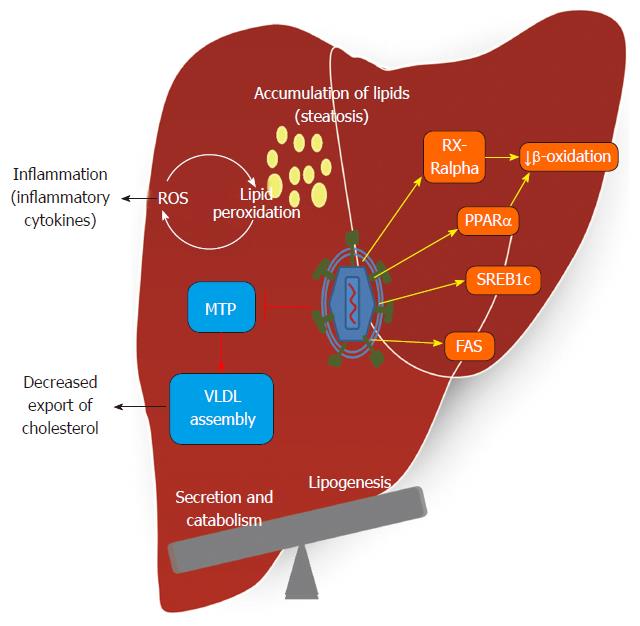
Figure 3 Hepatitis C virus effect in lipid metabolism and development of steatosis.
Hepatitis C virus (HCV) alters intracellular lipid metabolism to create an environment rich in lipids to facilitate its replication. This allows the accumulation of lipids, decrement in exportation of very low density lipoprotein (VLDL) and development of steatosis, a pathological phenotype associated with HCV chronic infection. Reactive oxygen species (ROS) generated during infection cause lipid peroxidation triggering inflammation. MTP: Microsomal triacylglycerol transfer protein; RXRα: Retinoid X receptor-alpha; PPARα: Peroxisome proliferators-activated receptor alpha; SREB1c: cholesterol regulatory element binding protein-1c; FAS: Fatty acid synthase.
- Citation: Fierro NA, Gonzalez-Aldaco K, Torres-Valadez R, Martinez-Lopez E, Roman S, Panduro A. Immunologic, metabolic and genetic factors in hepatitis C virus infection. World J Gastroenterol 2014; 20(13): 3443-3456
- URL: https://www.wjgnet.com/1007-9327/full/v20/i13/3443.htm
- DOI: https://dx.doi.org/10.3748/wjg.v20.i13.3443