Copyright
©2008 The WJG Press and Baishideng.
World J Gastroenterol. Dec 28, 2008; 14(48): 7309-7320
Published online Dec 28, 2008. doi: 10.3748/wjg.14.7309
Published online Dec 28, 2008. doi: 10.3748/wjg.14.7309
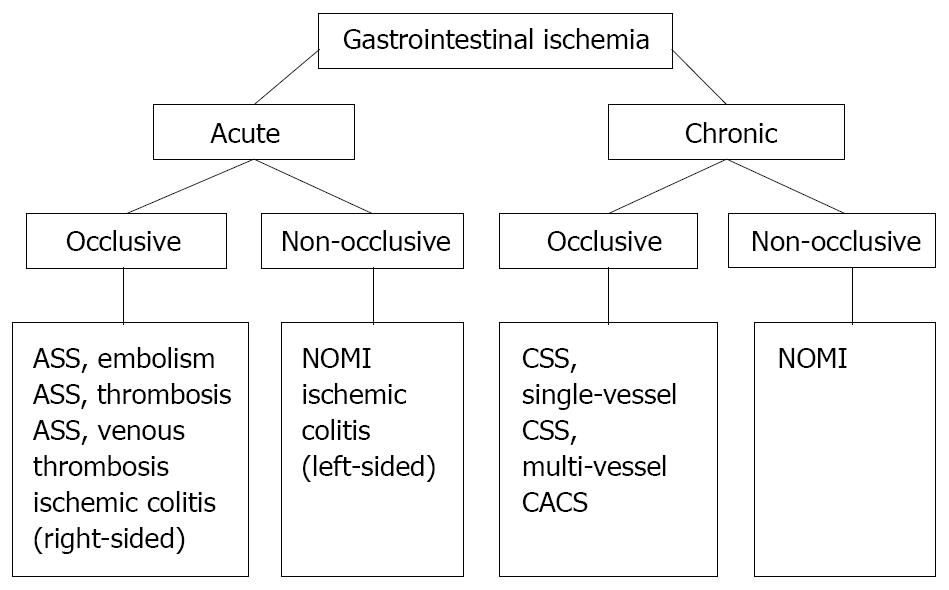
Figure 1 Classification of splanchnic, or gastrointestinal ischemia.
ASS: Acute splanchnic syndrome; CSS: Chronic splanchnic syndrome; CACS, Celiac artery compression syndrome; NOMI: Non-occlusive mesenteric ischemia.
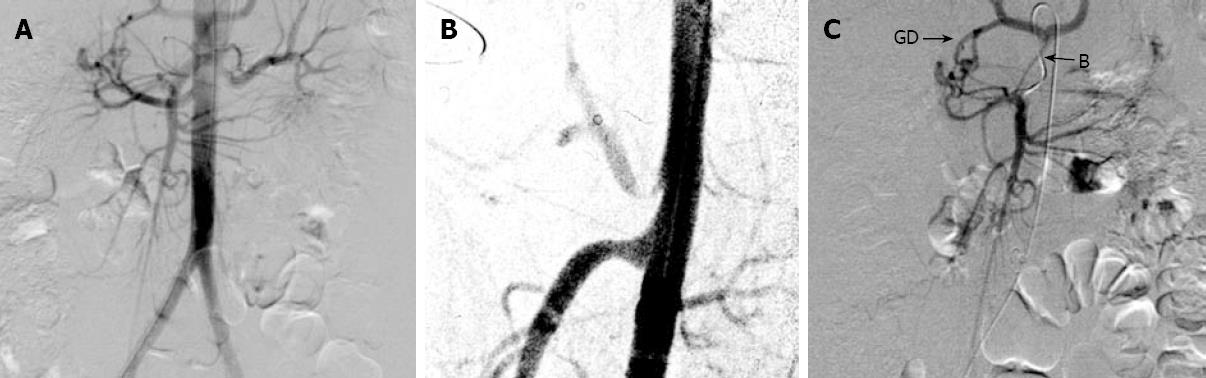
Figure 2 Collateral vessels: gastroduodenal (GD) artery and Buehlers artery (B).
A: The gastroduodenal (GD) artery and Buehlers artery (B) are visible on non-selective aortography indicating stenosis of the origin of either the CA or SMA. The late filling of the CA points to a stenosis in its origin; B: Lateral aortography showing an asymmetrical stenosis of the CA; C: On selective cannulation of the SMA, both collaterals are more clearly visible.
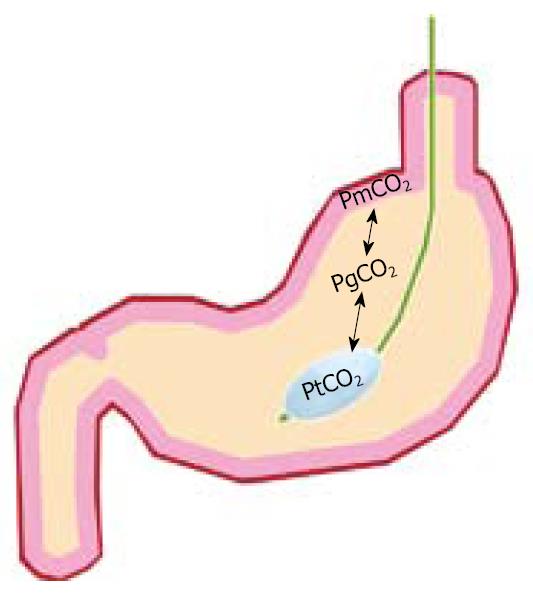
Figure 3 Tonometer balloon placed in the stomach nasogastrically.
CO2 diffuses rapidly over different membranes, therefore the tonometer PCO2 (PtCO2) will be in equilibrium with gastric luminal PCO2 (PgCO2) and mucosal PCO2 (PmCO2). The PCO2 can be measured from the catheter either from injected saline using blood gas analyzers or by connection to a semi-automated Tonocap device. The underlying physiological principle is that ischemia is always associated with PCO2 increase. Therefore, focal measurement of ischemia is possible for long periods via a minimally invasive technique.
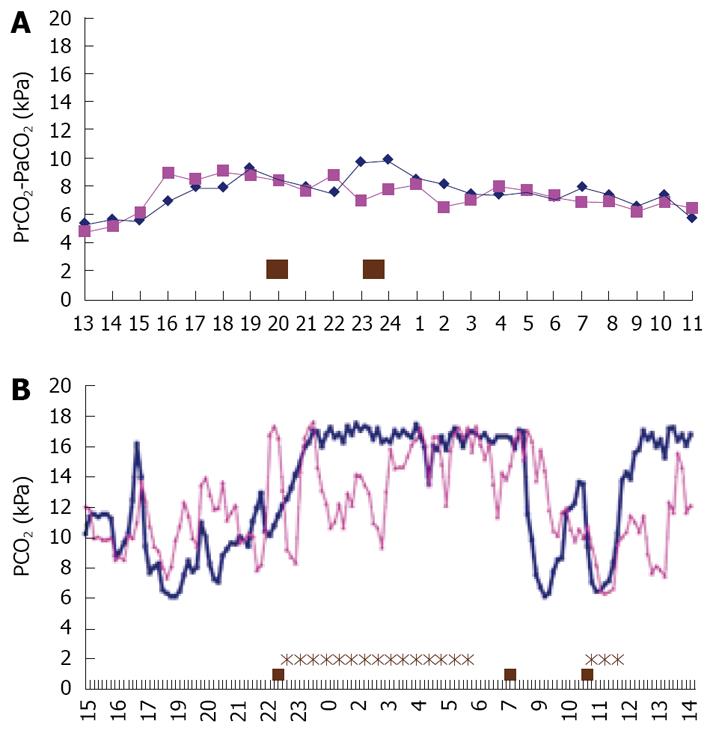
Figure 4 Imminent ASS and normal gastric and jejunal PCO2 pattern.
A: Normal 24 h PCO2 pattern in the stomach (squares) and jejunum (diamonds) with variation in PCO2, but no peaks above 11 kPa following meals; B: Imminent bowel infarction in a patient with severe 3 vessel CSS. After her evening meal she had pain for almost 6 h, and extreme ischemia with PCO2 > 16 kPa for 7 h. She was treated with endovascular stent placement the day after this measurement, with immediate relief of complaints. She is still doing well, over 3 years later.
- Citation: Kolkman JJ, Bargeman M, Huisman AB, Geelkerken RH. Diagnosis and management of splanchnic ischemia. World J Gastroenterol 2008; 14(48): 7309-7320
- URL: https://www.wjgnet.com/1007-9327/full/v14/i48/7309.htm
- DOI: https://dx.doi.org/10.3748/wjg.14.7309