Published online May 26, 2024. doi: 10.12998/wjcc.v12.i15.2678
Revised: April 3, 2024
Accepted: April 10, 2024
Published online: May 26, 2024
Radiological studies play a crucial role in the evaluation of patients with biliary duct obstruction, allowing for the guidance of clinical diagnosis towards a malignant or stone-induced etiology through the recognition of relevant imaging features, which must be continuously revisited given their prognostic significance. This article aims to emphasize the importance of recognizing crucial imaging aspects of malignant and stone-induced biliary obstruction.
Core Tip: Recognizing the radiological aspects of biliary obstruction is crucial for distinguishing between lithiasis and malignant origins, thereby facilitating the diagnosis and management of this pathology.
- Citation: Lindner C. Imaging features of malignant vs stone-induced biliary obstruction: Aspects to consider. World J Clin Cases 2024; 12(15): 2678-2681
- URL: https://www.wjgnet.com/2307-8960/full/v12/i15/2678.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v12.i15.2678
I read with great interest the letter written by Aydin and Irgul[1]. In their article, they aim to highlight some imaging findings for distinguishing between malignant biliary obstruction and common stone biliary obstruction.
I agree with Aydin and Irgul[1] that imaging studies play an invaluable role in the evaluation of patients with biliary tract obstruction. In the same line, I intend to contribute to the article highlighting some crucial imaging features of biliary obstruction that we should consider.
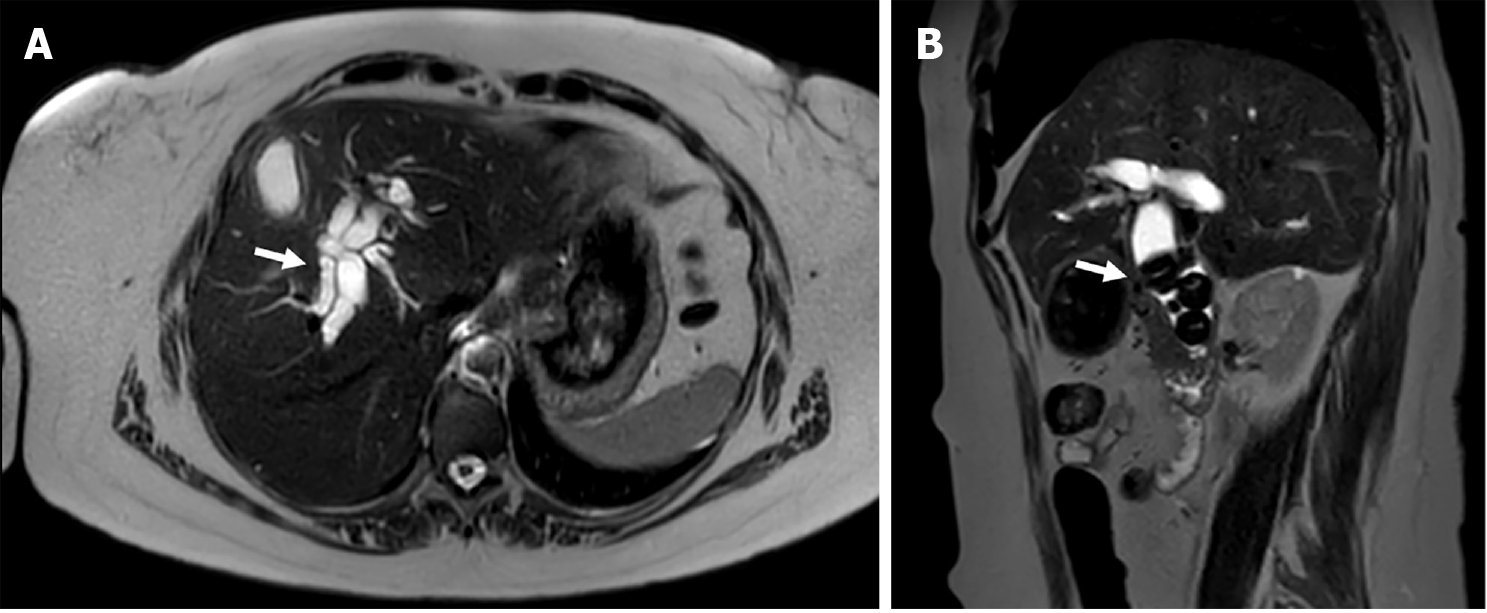
Obstruction of the biliary tree can occur as a result of gallstones disease[2] (Figure 1), as well as multiple types of cancers, including primary tumors originated from bile duct cells as well as those originating from adjacent organs that could cause extrinsic compression of the common bile duct (CBD), such as cholangiocarcinoma and pancreatic cancer respectively[3].
As expected, patients with biliary obstruction of malignant origin have a significantly worse clinical course compared to those with lithiasic obstruction of the bile duct, present a higher incidence of severe acute cholangitis, greater admission to critical care units, and 30-d mortality, as recently reported by Tsou et al[4], which underscores the impor
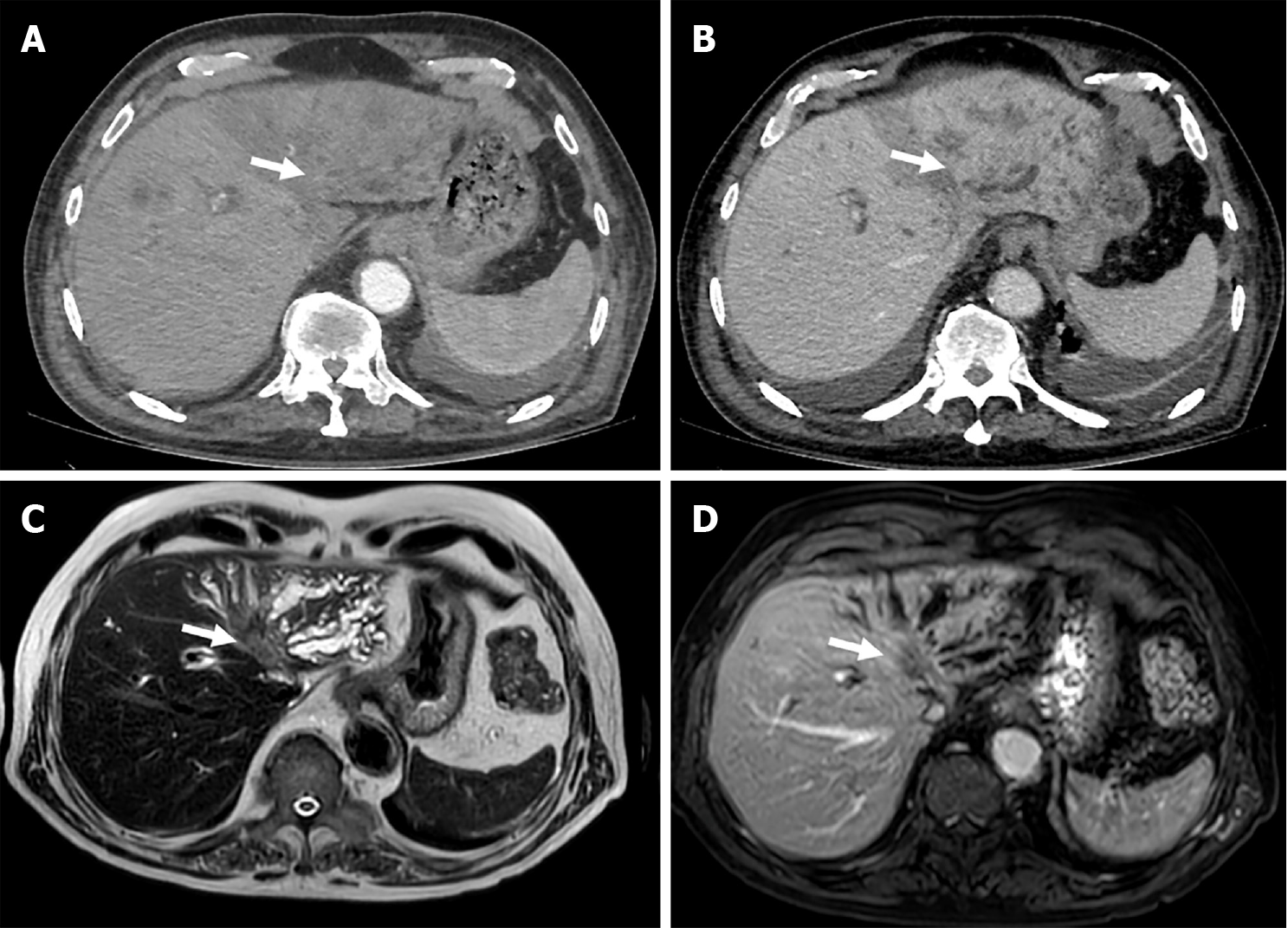
For instance, initial imaging evaluation of patients with biliary obstruction may depict dilatation of the CBD and common hepatic duct associated with heterogeneous sizeable non-encapsulated heterogeneous mass of irregular contour, accompanied by hepatic capsular retraction and dilated peripheral bile ducts, with progressive enhancement in delayed phases and slight-to high signal intensity on T2-weighted images (T2WI), and low signal intensity on T1-weighted images (T1WI), which is highly suggestive of primary bile duct carcinomas[3,5] (Figure 2).
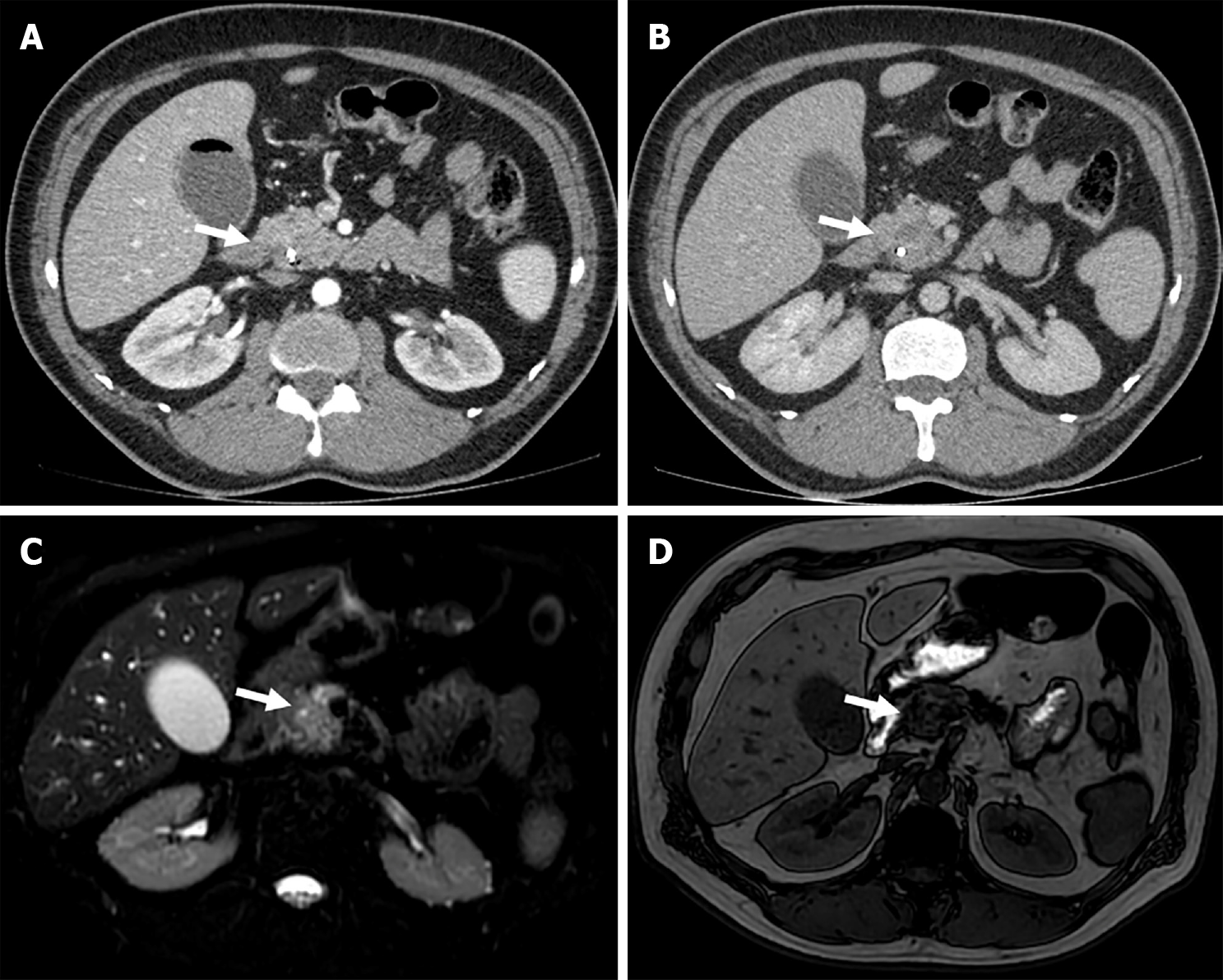
In addition, CBD dilation may also be associated with the presence of a heterogeneous enhancing mass dependent on the pancreatic head, with iso- to slightly hyperintense signal on T2WI, and hypointense signal on T1WI, which generates extrinsic compression of the CBD, which may produce secondary cholangitis[6] (Figure 3).
In both cases, the additional finding of focal hypovascular liver lesions with a peripheral halo and perihilar and retroperitoneal lymphadenopathy further support the diagnosis of biliary obstruction towards a malignant origin[7,8].
In summary, when conducting radiological evaluations of patients with bile duct obstruction, comprehensive consideration should be given to various imaging findings, with a focus on analyzing important imaging information. Considering the clinical implication of these diseases, I hope the discussion on the interesting articles by Tsou et al[4]. and Aydin and Irgul[1] will promote the permanent ongoing review of the imaging features of malignant and stone-induced bile duct obstruction to further improve the early recognition and appropriate management of these patients.
Provenance and peer review: Invited article; Externally peer reviewed.
Peer-review model: Single blind
Specialty type: Medicine, research and experimental
Country/Territory of origin: Chile
Peer-review report’s classification
Scientific Quality: Grade C
Novelty: Grade C
Creativity or Innovation: Grade C
Scientific Significance: Grade C
P-Reviewer: Bai H, China S-Editor: Liu H L-Editor: A P-Editor: Yu HG
| 1. | Aydin S, Irgul B. Response letter to "Acute cholangitis: Does malignant biliary obstruction vs choledocholithiasis etiology change the outcomes?" with imaging aspects. World J Clin Cases. 2024;12:1029-1032. [PubMed] [DOI] [Cited in This Article: ] [Reference Citation Analysis (0)] |
| 2. | Duhancioglu G, Arif-Tiwari H, Natali S, Reynolds C, Lalwani N, Fulcher A. Traveling gallstones: review of MR imaging and surgical pathology features of gallstone disease and its complications in the gallbladder and beyond. Abdom Radiol (NY). 2024;49:722-737. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 1] [Reference Citation Analysis (0)] |
| 3. | Katabathina VS, Dasyam AK, Dasyam N, Hosseinzadeh K. Adult bile duct strictures: role of MR imaging and MR cholangiopancreatography in characterization. Radiographics. 2014;34:565-586. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 80] [Cited by in F6Publishing: 58] [Article Influence: 6.4] [Reference Citation Analysis (0)] |
| 4. | Tsou YK, Su YT, Lin CH, Liu NJ. Acute cholangitis: Does malignant biliary obstruction vs choledocholithiasis etiology change the clinical presentation and outcomes? World J Clin Cases. 2023;11:6984-6994. [PubMed] [DOI] [Cited in This Article: ] [Cited by in F6Publishing: 1] [Reference Citation Analysis (0)] |
| 5. | Joo I, Lee JM, Yoon JH. Imaging Diagnosis of Intrahepatic and Perihilar Cholangiocarcinoma: Recent Advances and Challenges. Radiology. 2018;288:7-13. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 90] [Cited by in F6Publishing: 93] [Article Influence: 15.5] [Reference Citation Analysis (0)] |
| 6. | Schawkat K, Manning MA, Glickman JN, Mortele KJ. Pancreatic Ductal Adenocarcinoma and Its Variants: Pearls and Perils. Radiographics. 2020;40:1219-1239. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 15] [Cited by in F6Publishing: 31] [Article Influence: 7.8] [Reference Citation Analysis (0)] |
| 7. | Costello JR, Kalb B, Chundru S, Arif H, Petkovska I, Martin DR. MR imaging of benign and malignant biliary conditions. Magn Reson Imaging Clin N Am. 2014;22:467-488. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 12] [Cited by in F6Publishing: 8] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 8. | Kim DW, Kim SY, Yoo C, Hwang DW. Update on Biliary Cancer Imaging. Radiol Clin North Am. 2022;60:825-842. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 1] [Cited by in F6Publishing: 1] [Article Influence: 0.5] [Reference Citation Analysis (0)] |