Published online May 26, 2024. doi: 10.12998/wjcc.v12.i15.2586
Revised: February 28, 2024
Accepted: April 7, 2024
Published online: May 26, 2024
Bronchogenic cysts are rare developmental anomalies that belong to the category of congenital enterogenous cysts. They arise from lung buds and are present at birth. The embryonic foregut is their origin. Typically, they are located within the chest cavity, particularly in the cavum mediastinale of the thoracic cavity or lodged in the pulmonary parenchyma, and are considered a type of lung bud malformation.
A 49-year-old male patient was admitted to the hospital due to the detection of a retroperitoneal mass during a physical examination. Two weeks before admission, the patient underwent a physical examination and routine laboratory tests, which revealed a space-occupying mass in the retroperitoneal region. The patient did not report any symptoms (such as abdominal pain, flatulence, nausea, vomiting, high fever, or chills). The computed tomography (CT) revealed a retroperitoneal space-occupying lesion with minimal enhancement and a CT value of approximately 36 Hounsfield units. The lesion was not delineated from the boundary of the pancreatic body and was closely related to the retroperitoneum locally.
Following a series of tests, an abdominal mass was identified, prompting the implementation of a laparoscopic retroperitoneal mass excision procedure. During the investigation, an 8 cm × 7 cm cystic round-shaped mass with a distinct demarcation was identified in the upper posterior region of the pancreas. Subsequently, full resection of the mass was performed. Postoperative pathological examination reveled a cystic mass characterized by a smooth inner wall. The cystic mass was found to contain a white, viscous liquid within its capsule.
Core Tip: A 49-year-old male with no significant medical or family history was diagnosed with a retroperitoneal mass during a routine physical examination, despite showing no typical symptoms. The absence of common diseases such as hypertension or diabetes in his medical history, with normal physical examination and laboratory results, highlighted the unusual nature of this case. The mass, detected incidentally, underscoreds the importance of routine health checks in identifying potentially serious conditions in asymptomatic patients. This case emphasizes the critical role of comprehensive evaluations and the need for surgical intervention in managing unexpected findings, demonstrating the value of caution in routine medical examinations.
- Citation: Malik A, Naseer QA, Iqbal MA, Han SY, Dang SC. Retroperitoneal bronchogenic cyst: A case report and review of literature. World J Clin Cases 2024; 12(15): 2586-2596
- URL: https://www.wjgnet.com/2307-8960/full/v12/i15/2586.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v12.i15.2586
Bronchogenic cysts originate from the foregut and are most commonly situated in the mediastinum, as noted previously[1,2]. However, these cystic anomalies have also been identified in less common locations, including the esophagus, as reported by Altieri et al[1] and near the diaphragm[3,4]. While often presenting without symptoms, these cysts may lead to clinical concerns through infection or by exerting pressure on adjacent anatomical structures, as described previously[2]. To mitigate such issues and avert further complications, surgical removal of the cysts is frequently advocated[2]. While these cysts are generally asymptomatic, they can become infected or exert compressive effects on adjacent tissues[2]. This case study describes a case involving a subdiaphragmatic retroperitoneal bronchogenic cyst, with a definitive diagnosis established through histopathological examination of the surgically excised specimen.
A retroperitoneal mass was identified during a routine physical examination. The mass was detected two weeks prior to his admission, through physical assessment and standard laboratory tests.
A 49-year-old male who was hospitalized following a routine physical examination unexpectedly revealed a retroperitoneal mass despite the absence of symptoms such as nausea, vomiting, fever, abdominal pain, or distension.
The patient's medical history was devoid of any conditions, including the absence of other diseases such as hypertension (HTN), diabetes mellitus (DM), heart disease, or tuberculosis (TB).
The patient reported no family history of any disease or cancerous growth.
During the physical examination, the patient's abdominal area exhibited a flat and soft appearance, without any indications of gastrointestinal problems or peristaltic movements. Moreover, there were no signs of varices in the abdominal wall, tenderness, rebound pain, or muscle guarding. The liver and spleen displayed normal characteristics, and Murphy's sign elicited a negative response. No pain was elicited during percussion in the liver and kidney regions, and no anomalies were detected during digital rectal examination. The vital signs of the patient were recorded as follows: Body temperature of 36.2 ℃, arterial blood pressure of 130/65 mmHg, SpO2 level of 95%, pulse rate of 105 beats per minute, and respiration rate of 19 breaths per minute. In general, the findings of the physical examination were within normal limits.
Laboratory analyses revealed a C-reactive protein concentration of 24.0 mg/L, a white blood cell (WBC) count of 12.4 × 109/L, and a neutrophil proportion of 77.6%. The results of the endocrine assessment conducted to evaluate excessive adrenal secretion revealed no abnormalities, as shown in Table 1. Blood biochemistry results fell within the normal range, and after comprehensive laboratory analyses and a thorough physical examination, there were no evident contraindications for the surgical extraction of the tumor.
| Actual parameter | Amount of concentration | Reference values |
| Leukocyte (WBC), × 109/L | 6.1 | 3.5-9.5 |
| Neutrophils, × 109/L | 2.6 | 1.8-6.3 |
| Lymphocytes, × 109/L | 2.6 | 1.1-3.2 |
| Monocytes, × 109/L | 0.7 | 0.1-0.6 |
| Eosinophils, × 109/L | 0.12 | 0.02-0.52 |
| Basophil, × 109/L | 0.07 | 0-0.06 |
| CA19-9, U/mL | 3.3 | < 37.0 |
| CEA, ng/mL | 2.3 | < 5.0 |
| AFP, ng/mL | 1.25 | < 8.78 |
| CA125, U/mL | 6.1 | < 35 |
Table 1 presents the results of a series of presurgery laboratory tests conducted on the patient. It provides the actual values of various measured parameters, their corresponding normal reference values, and the units of measurement. The first parameter in the table is the leukocyte or WBC count, which measures the total WBCs in the bloodstream. The patient's WBC count was determined to be 6.1 × 109/L, and this value falls within the typical reference range of 3.5-9.5 × 109/L. Additionally, the table includes various types of WBCs, such as neutrophils, lymphocytes, monocytes, eosinophils, and basophils. The patient's neutrophil count was slightly below the standard range, while the lymphocyte count was within the normal reference range. The counts of the other types of WBCs all fell within their respective normal ranges. Additionally, the table reports the values of four tumor markers: Carbohydrate antigen (CA)19-9, carcinoembryonic antigen (CEA), alpha-fetoprotein (AFP), and CA125. Tumor markers are substances produced either by cancer cells or by normal cells in response to cancer. They serve the purpose of detecting cancer, monitoring its progression, and evaluating treatment efficacy. In this particular case, all four tumor markers were within their normal reference ranges, signifying the absence of evidence for cancer.
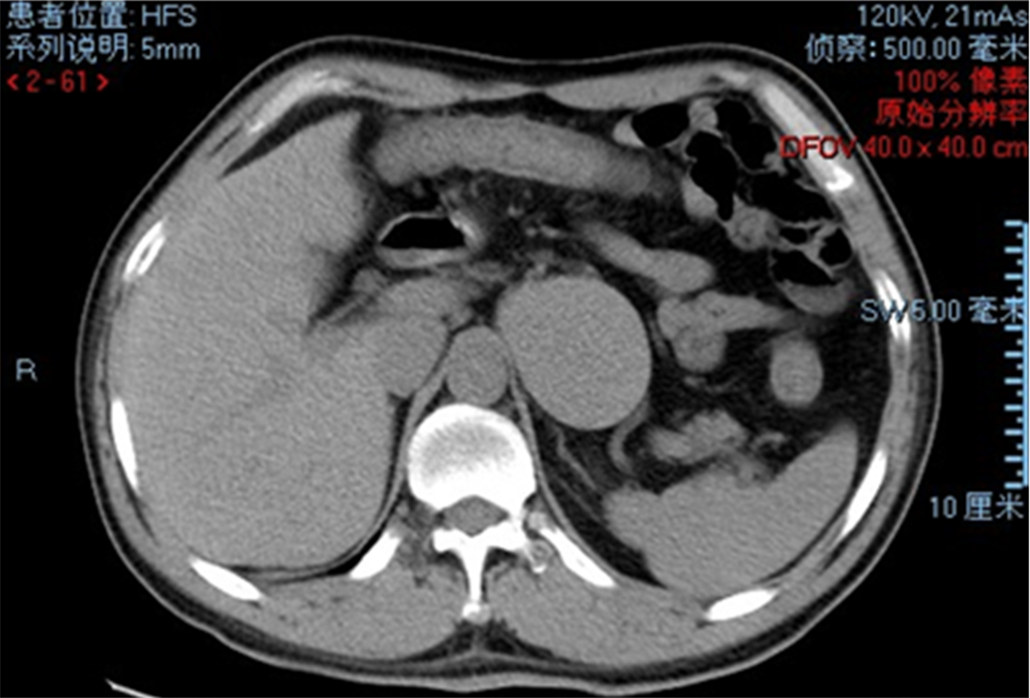
Further diagnostic evaluations were undertaken through noncontrast computed tomography (CT) scans to characterize the retroperitoneal space-occupying lesion. Imaging revealed that the lesion demonstrated characteristics suggestive of limited enhancement, an observation attributable to the imaging technique employed. The cyst content was noted to have a uniform density, with CT values ranging between 17 and 36 Hounsfield units, which are indicative of the lesion composition. A notable finding was the increased thickness of the cyst wall, a feature that may suggest underlying contamination or inflammation. Figure 1 shows the anatomical location of an oval cystic lesion situated at the posterior lower aspect of the left lateral lobe of the liver, within the retroperitoneal space, adjacent to the right side of the spine, and to the left of the inferior vena cava. However, it is important to clarify that the figure predominantly shows a large cystic mass accompanied by scattered calcifications within the abdominal-pelvic cavity, without distinct demarcation of the specific lesion across the mentioned anatomical landmarks.
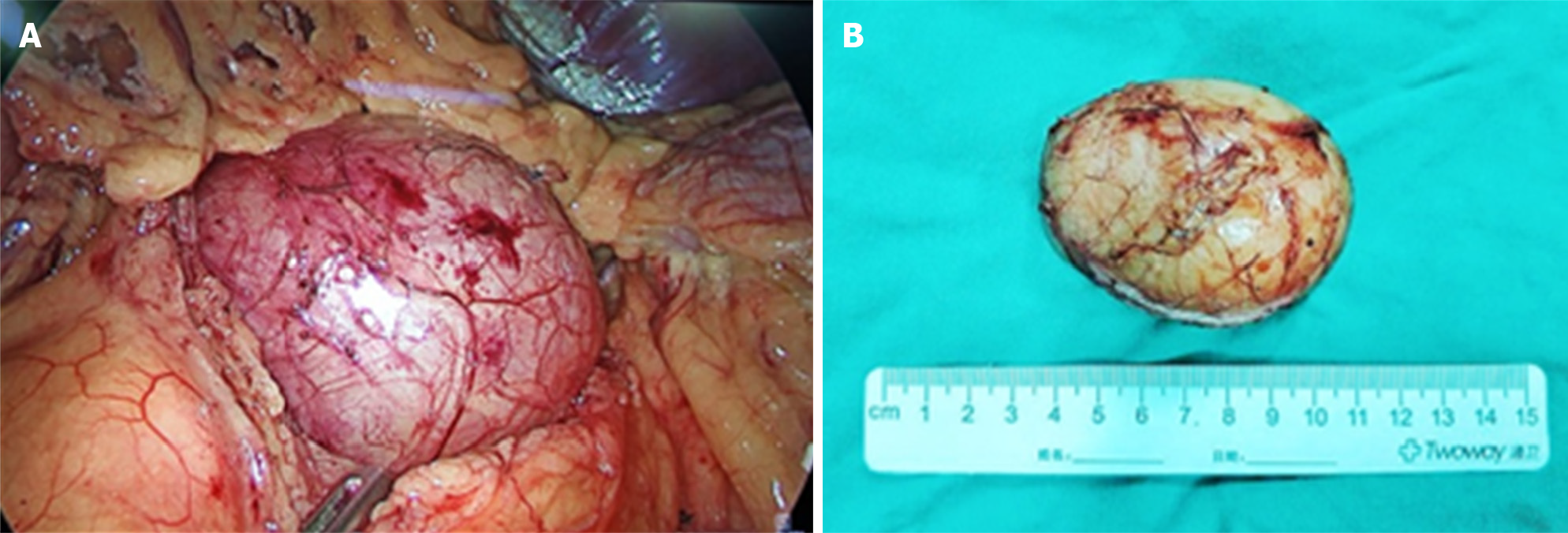
Upon identifying an unexpected retroperitoneal mass during a standard physical examination, the 49-year-old male was subjected to a noncontrast CT scan, which delineated a lesion with limited enhancement and a uniform density, alongside an increased cyst wall thickness, suggesting possible underlying issues. The decision for surgical intervention was made, leading to the laparoscopic resection of the mass. Intraoperatively, the lesion, located on the dorsal side of the upper pole of the left kidney, was noted for its soft, gray-yellow appearance with a smooth surface. The tumor was characterized as soft and gray-yellow and had a smooth surface, and it was successfully completely excised. Upon opening the mass, a thick, jelly like substance was found within, and the thickness of the capsule wall measured approximately 0.2 cm, as shown in Figure 2A. The resected specimen, measuring 8.8 cm × 7.2 cm × 2.6 cm, underwent histopathological examination, which confirmed the diagnosis of a retroperitoneal bronchogenic cyst (Figure 2B). This examination revealed a cystic mass with a smooth inner wall, containing white viscous fluid, and a capsule wall lined with pseu
Considering the patient's clinical presentation and subsequent investigative findings, the final diagnosis was determined to be a retroperitoneal bronchogenic cyst.
The patient was treated through laparoscopic resection of the retroperitoneal lesion under general anesthesia, successfully excising the cystic lesion. Postoperative recovery was uneventful, leading to discharge five days after the procedure without any complications.
The surgical procedure was carried out successfully, and the patient was safely transferred to the hospital ward without any postoperative complaints. Subsequent laboratory results indicated a reduction in C-reactive protein levels and WBC count, with a recorded value of 6.1-9 mg/L, while the neutrophil percentage remained at 77.6%. The patient's condition remained stable, characterized by normal vital signs, satisfactory overall well-being, restful sleep, and a positive mental state. Examination of the abdomen did not reveal any tenderness, and bowel sounds were within the expected range. After a postoperative recovery period of five days, the patient exhibited excellent progress without any complications, which ultimately led to their discharge from the hospital.
Bronchogenic cysts are a type of congenital developmental anomaly that typically occurs in the mediastinum but can also occur in other areas, such as the abdominal cavity, skin, and diaphragm. Retroperitoneal bronchogenic cysts are frequently observed in the left adrenal region and frequently exhibit an absence of symptoms, hence contributing to the potential for misdiagnosis[5]. It is crucial to distinguish these cysts from other conditions, such as adrenal adenomas, renal cysts, and cystic teratomas. As a consequence of the initial findings, the patient was referred to the surgical department for further evaluation and medical intervention. Throughout the illness, the patient did not manifest any distressing symptoms, such as abdominal pain, abdominal distension, diarrhea, hematuria, urinary pain, frequent urination, cold sensitivity, fever, night sweats, cough, or hemoptysis. Both urinary and bowel functions were reported to be normal, and no significant recent weight loss was documented. Furthermore, the patient had no previous medical history of conditions such as HTN, DM, heart disease, or TB. This case report highlights the discovery of a retroperitoneal space-occupying lesion in a patient who exhibited no accompanying symptoms. Imaging findings suggested the presence of additional cystic lesions within the retroperitoneal region, necessitating further inquiries to establish an accurate diagnosis and develop a suitable course of treatment for this individual.
There were no indications of varices, tenderness, rebound pain, or muscle guarding. Both the liver and spleen appeared normal. Percussion in the liver and kidney areas did not elicit any pain, and digital rectal examination revealed no abnormalities. Overall, the physical examination findings were within normal parameters.
Laboratory tests showed a C-reactive protein level of 24.0 mg/L, a WBC count of 12.4 × 109/L, and a neutrophil percentage of 77.6%. Endocrine evaluation for excessive adrenal secretion revealed no abnormalities (Table 1). A CT scan revealed a retroperitoneal mass without significant enhancement. While the diagnosis confirmed the presence of an abdominal mass, further pathological assessment was needed for precise characterization. Blood biochemistry results were normal. After thorough laboratory analyses and physical examination, there were no contraindications for surgical tumor removal. Surgery was scheduled following appropriate preoperative assessments.
Bronchogenic cysts can be categorized into three types based on their location: Intrapulmonary, mediastinal, and ectopic. The mediastinal type is the most prevalent and typically manifests as a clearly defined cystic structure in the posterior mediastinum. Ectopic variants, which can appear in locations such as the neck, brain, and spinal dura, are rare and may occasionally be found in the retroperitoneal area. Retroperitoneal bronchogenic cysts are exceedingly rare, with only sixty-two cases reported in the medical literature. Among these cases, approximately thirty were verified as genuine retroperitoneal bronchogenic cysts based on anatomical and pathological criteria[6]. Retroperitoneal bronchogenic cysts are an uncommon, accounting for only 0.03% of the tumor incidence. These cysts are thought to have their origins in the embryonic foregut and arise from a segment of the abnormally developed trachea and bronchial tree that takes shape in the early stages following the detachment and implantation of the plumule in the abdominal cavity[5,7]. The concept posits a potential correlation between the occurrence of retroperitoneal bronchogenic cysts on the left side of the body and the separation of the plumule from the left side after anterior bowel transposition. Retroperitoneal bronchogenic cysts are a rare clinical discovery, and most of these lesions typically cluster around the left adrenal gland. The peripancreatic area is the second most frequently affected site for these cysts and can occasionally be mistaken for adenomas during preoperative imaging[8,9]. We examined a patient with a congenital malformation in the posterior mediastinum, likely attributed to the abnormal development of the foregut. One of the retroperitoneal cysts initially appeared as a left adrenal cyst and was effectively excised using laparoscopic techniques. The cyst was definitively diagnosed as a bronchogenic cyst through pathological analysis, highlighting the need to consider bronchogenic cysts as a possible diagnosis for retroperitoneal cysts.
Retroperitoneal bronchogenic cysts generally remain asymptomatic unless complications such as infection or significant enlargement leading to the compression of neighboring organs arise. The usual indications may involve unexplained abdominal swelling and a sense of fullness before lunchtime. In certain instances, when the adrenal glands are compressed, symptoms resembling those associated with pheochromocytoma have been documented. Early diagnosis and prompt treatment are crucial for preventing potential complications, as elevated levels of hormones may be released if left untreated[10,11]. Retroperitoneal bronchogenic cysts exhibit a nearly equal distribution between genders, affecting both women and men. Approximately 82% of these cysts are observed to localize on the left side of the abdominal region[12]. Bronchogenic cysts situated in deep anatomical locations, such as the posterior pelvic peritoneum, pose significant challenges in preoperative identification and are commonly subject to misdiagnosis[13]. The patient underwent a laparoscopic resection procedure for the retro-abdominal lesion under general anesthesia. No ascites was detected in the pelvic cavity, and there were no apparent abnormalities in various abdominal organs, including the liver, stomach, lungs, glands, spleen, small intestine, large intestine, and pelvic cavity. During the operation, the tumor was located on the dorsal side of the upper pole of the left kidney, as illustrated in Figure 2A.
Symptoms such as sickness, vomiting, and stomach discomfort may be useful in obtaining a diagnosis through medical assessment if the lesions become substantial enough to compress neighboring organs. While CT and magnetic resonance imaging are valuable diagnostic modalities for retroperitoneal bronchogenic cysts, the process of establishing a definitive diagnosis can be complex due to various aspects, including the protein or calcium composition of the cysts, their dimensions, compaction, or the potential occurrence of infection[8,14,15]. The tumor was characterized as soft and gray-yellow and had a smooth surface, and it was successfully completely excised. Upon opening the mass, a thick, jelly like substance was found within, and the thickness of the capsule wall measured approximately 0.2 cm, as shown in Figure 2B.
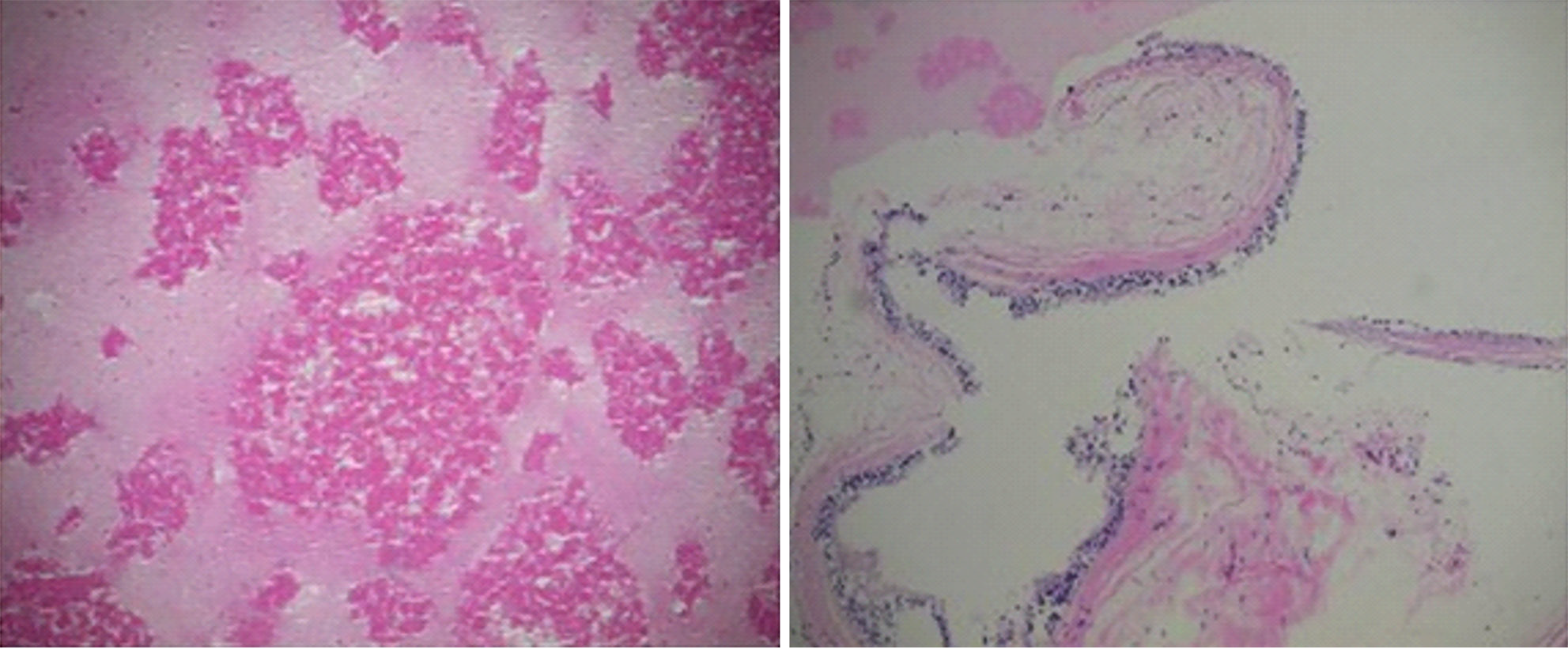
The retroperitoneal bronchogenic cyst was established during the postoperative pathological examination. The mass exhibited a rounded shape, measuring approximately 8 cm × 7 cm, and had a soft consistency with an intact capsule. Microscopic examination of the specimen revealed a cystic mass with a smooth inner wall, containing white viscous fluid. The capsule wall was lined with pseudostratified ciliated columnar epithelium and included glands, cartilage, and smooth muscle. The pathological diagnosis confirmed tha the mass was as a bronchogenic cyst, as depicted in Figure 3.
Following a successful surgical procedure, the patient was transferred safely to the hospital ward without experiencing any postoperative issues. Subsequent laboratory results showed decreased C-reactive protein levels and WBC counts, with a recorded range of 6.1-9 mg/L, while the neutrophil percentage remained stable at 77.6%. The patient's condition remained stable, with normal vital signs, satisfactory overall well-being, restful sleep, and a positive mental state. Abdominal examination revealed no tenderness, and bowel sounds were normal. After a 5-d postoperative recovery period, the patient made excellent progress without complications, leading to discharge from the hospital. Surgical removal is typically the treatment of choice, and symptoms of this lesion type often improve following surgical intervention. Fifty percent of all retroperitoneal bronchogenic cysts are discovered incidentally[8].
During sonogram investigation, retroperitoneal cystic lesions typically present as anechoic lesions with or without echo fragmentation. Computerized axial tomography typically indicates a thin-walled, well-defined lesion with low water density and little enhancement, although these lesions may have high density due to protein content, hemorrhagic content, or sticky mucinous tissue. Fluid level and wall calcification may also beobserved[6]. Retroperitoneal cystic lesions have a wide range of possible causes, including adrenal cysts, pancreatic pseudocysts, teratomas, and cystic lymphangiomas. Bronchogenic cysts are treated surgically and have a very good long-term success rate[2,12].
The use of endoscopic ultrasound (EUS) seems to exhibit a higher level of effectiveness compared to CT in the identification and characterization of retroperitoneal cystic masses. This is mostly due to its ability to provide a clear depiction of the mass itself, as well as the surrounding structures within the posterior peritoneal region. EUS-guided fine-needle aspiration is a diagnostic procedure that can be employed to ascertain the malignancy or benign nature of a lesion. There have been recorded instances of retroperitoneal bronchogenic cysts with notably increased levels of serum CA19-9, while the underlying cause for this increase remains unclear and requires additional investigation[16]. The use of serum CA19-9 measurement has the potential to provide valuable diagnostic information for the identification of retroperitoneal bronchogenic cysts[17]. Retroperitoneal bronchogenic cysts were first described by Miller et al[18] in 1953 and are considered to be extremely rare. A thorough examination of the PubMed database has shown a total of 88 recorded cases of retroperitoneal bronchogenic cysts in the global English-language literature from 1991 to 2022. In the context of this study, a comprehensive analysis was conducted on a total of 40 publications, each presenting detailed information on 45 cases involving the laparoscopic extraction of red blood cells. The evaluation encompassed the entirety of the texts as well as the pathological findings associated with these cases. Table 2 provides a concise summary of the papers that are included for reference.
| Country | Year | Age (yr) | Sex | Location | Size (cm) | Chief complaint | Surgical technique | First author | Ref. |
| Japan | 1997 | 24 | F | L adrenal gland | 3 | Asymptomatic | Laparoscopic | Tokuda N | [19] |
| Japan | 1998 | 49 | F | R adrenal gland | 3.2 × 2.2 | Asymptomatic | Laparoscopic | Yamamoto E | [23] |
| Australia | 2002 | 15 | M | L adrenal gland | 5.5 × 3.5 × 1.2 | L flank pain | Laparoscopic | McCrystal DJ | [24] |
| Australia | 2002 | 8 | F | L adrenal gland | 4 × 3 × 2 | Abdominal pain | Laparoscopic | McCrystal DJ | [24] |
| United States | 2003 | 59 | F | L adrenal gland | 7 × 5 | Asymptomatic | Laparoscopic | Hedayati N | [25] |
| Japan | 2003 | 41 | F | L adrenal gland | 9.2 | L flank pain | Laparoscopic | Ishikawa T | [26] |
| Japan | 2004 | 36 | M | L adrenal gland | 5 × 3 | Asymptomatic | Laparoscopic | Ishizuka O | [27] |
| United States | 2007 | 75 | F | L adrenal gland | 5 | Abdominal pain | Laparoscopic | Terry NE | [28] |
| China | 2007 | 55 | M | L adrenal gland | 4 × 3 | Asymptomatic | Laparoscopic | Chu PY | [29] |
| Japan | 2007 | 39 | M | L adrenal gland | 3.5 × 3 | Fever | Laparoscopic | Minei S | [30] |
| United States | 2008 | 40 | M | L adrenal gland | 6.2 | Asymptomatic | Laparoscopic | Roma A | [31] |
| Korea | 2009 | 41 | F | L adrenal gland | 4.8 × 3.5 × 4.2 | Asymptomatic | Laparoscopic | Chung JM | [12] |
| United States | 2009 | 67 | M | L upper-quadrant | 3.9 × 3.7 | Asymptomatic | Laparoscopic | Obando J | [32] |
| Portland | 2010 | 44 | M | L adrenal gland | 3 | Asymptomatic | Laparoscopic | El Youssef R | [33] |
| Japan | 2010 | 64 | F | Stomach posterior wall | 3 × 4 × 2 | Asymptomatic | Laparoscopic | Inaba K | [34] |
| Spain | 2010 | 67 | M | Gastro-esophageal junction | 6 | Low back pain | Laparoscopic | Díaz Nieto R | [35] |
| United States | 2012 | 23 | F | R adrenal gland | 4 | Asymptomatic | Robotic | Alguraan Z | [36] |
| United States | 2012 | 23 | F | L adrenal gland | 5.2 × 4 | Abdominal discomfort | Laparoscopic | O'Neal PB | [37] |
| Germany | 2013 | 50 | M | L adrenal gland | 4 | L flank pain | Laparoscopic | Jannasch O | [38] |
| China | 2013 | 50 | F | Pancreas posterior wall | 3 | L flank pain | Laparoscopic | Cai Y | [39] |
| Switzerland | 2013 | 42 | F | L adrenal gland | 5 × 3.6 × 4 | Epigastric pain | Laparoscopic | Runge T | [40] |
| Portugal | 2013 | 36 | F | L upper quadrant | 8 | Abdominal pain | Laparoscopic | Castro R | [41] |
| China | 2014 | 30 | F | L adrenal gland | 1.5 × 2 × 2 | Asymptomatic | Laparoscopic | Dong B | [42] |
| China | 2014 | 51 | M | L adrenal gland | 4.5 | Headache | Laparoscopic | Cao DH | [43] |
| Japan | 2014 | 27 | M | L adrenal gland | 5.4 × 3.8 | Asymptomatic | Laparoscopic | Terasaka T | [44] |
| China | 2015 | 8 | M | L adrenal gland | 4 | Asymptomatic | Laparoscopic | Zhang D | [45] |
| India | 2015 | 34 | F | R hypochondrium | 10 × 6 | R flank heavy | Laparoscopic | Trehan M | [46] |
| China | 2015 | 52 | M | L crus of the diaphragm | 2.5 × 2.5 × 0.5 | Asymptomatic | Laparoscopic | Jiang X | [47] |
| Türkiye | 2015 | 25 | F | L adrenal gland | 4 | L flank pain | Laparoscopic | Bulut G | [48] |
| Korea | 2015 | 57 | M | L adrenal gland | 4.8 × 2.5 | Asymptomatic | Laparoscopic | Yoon YR | [49] |
| China | 2017 | 48 | F | L adrenal gland | 8 × 6 × 5.5 | Epigastric pain | Laparoscopic | Wang M | [17] |
| China | 2018 | 78 | M | Inferior of the L renal vein, L side of IVC | 7 | Asymptomatic | Robotic | Liu Q | [50] |
| China | 2018 | 33 | M | L hepatic hilum | 4.5 | Asymptomatic | Robotic | Liu Q | [50] |
| Türkiye | 2018 | 38 | F | L adrenal gland | NA | L upper abdominal pain | Laparoscopic | Bolton JW | [51] |
| India | 2020 | 30 | M | L adrenal gland | 7 × 5 | Upper abdominal pain | Laparoscopic | Sinha V | [52] |
| China | 2020 | 33 | M | R adrenal gland | 3.1 × 5.9 | Asymptomatic | Laparoscopic | Wen Y | [53] |
| China | 2020 | 27 | M | L adrenal gland | 2.1 × 4.1 | Asymptomatic | Laparoscopic | Wen Y | [53] |
| China | 2021 | 41 | F | L adrenal gland | 3.5 × 3 | Lumbar back discomfort | Laparoscopic | Qingyu J | [54] |
| China | 2021 | 17 | F | L adrenal gland | 2.9 × 1.7 × 2.8 | Epigastric pain | Laparoscopic | Wu LD | [55] |
| China | 2021 | 53 | F | L adrenal gland | 3.3 × 2.7 × 3.5 | Back pain | Laparoscopic | Yuan K | [22] |
| New Zealand | 2021 | 39 | M | L adrenal gland | 3 | L flank pain | Laparoscopic | Cowan S | [56] |
| Japan | 2022 | 16 | F | Under the L diaphragm | 3.8 | Upper abdominal pain | Laparoscopic | Tadokoro T | [57] |
| China | 2022 | 27 | M | R adrenal gland | 3.6 × 3.5 × 3.4 | Asymptomatic | Laparoscopic | Hu BY | [58] |
| China | 2022 | 18 | M | L adrenal gland | 7.1 × 3.6 × 7 | Asymptomatic | Laparoscopic | Hu BY | [58] |
| China | 2022 | 6 | M | L adrenal gland | 4.5 × 2.8 × 8 | Abdominal pain | Laparoscopic | Hu BY | [58] |
Tokuda et al[19] reported the first laparoscopic resection of such cysts in 1997, with a focus on cysts up to 3 cm in size. It is worth noting that this particular surgical treatment has been predominantly documented in China, with 17 cases (37.8%). Subsequently, 8 cases were recorded in Japan (17.8%), while 6 cases were reported in the United States (13.3%). The observation of differences based on regional and racial factors is consistent with the findings reported by Liang et al[20]. Comprehensive literature reviews were sequentially conducted by Cetinkurşun et al[21], Liang et al[20], Govaerts et al[6], and Yuan et al[22] in the years 1997, 2005, 2012, and 2021, respectively. It is noteworthy to emphasize that the aforementioned research included a significant cohort of patients who underwent surgical procedures utilizing the open technique. After successful surgical resection and pathological confirmation of the bronchogenic cyst, comprehensive preoperative assessment, which plays a crucial role in guiding the surgical approach. Table 1 presents the results of a series of presurgery laboratory tests conducted on the patient, providing a detailed account of the patient's clinical status prior to the operation. This includes the actual values of various measured parameters, their corresponding normal reference values, and the units of measurement. Specifically, the leukocyte or WBC count, which measures the total WBCs in the bloodstream, was determined to be within the typical reference range, indicating no infection or inflammation. Additionally, the table reports the values of four tumor markers: CA19-9, CEA, AFP, and CA125, all of which are within their normal reference ranges, indication the absence of evidence for cancer. This comprehensive laboratory analysis, alongside a thorough physical examination, underscored the absence of contraindications for surgical extraction of the tumor, facilitating a well-informed decision to proceed with laparoscopic resection. Furthermore, our study was extended to incorporate the latest findings from the preceding 2 years and address any deficiencies that were not covered in previous enquiries. These collaborative endeavors resulted in consistent discoveries concerning the clinical attributes of the illness, including elements such as the age of the patients, initial symptoms, and prevalent anatomical sites of the cysts.
In summary, retroperitoneal bronchogenic cysts, while rare and often asymptomatic, are typically identified incidentally and best managed through surgical removal, with laparoscopic excision being the preferred method. The case discussed illustrates the successful laparoscopic resection of such a cyst, emphasizing the importance of a multidisciplinary approach for optimal diagnosis and management. The challenges in preoperative diagnosis due to the deep anatomical locations of cyst highlight the need for prompt intervention to prevent complications. The current literature supports the effectiveness of laparoscopic surgery, noting a favorable long-term prognosis without recurrence. Future research should focus on enhancing diagnostic techniques and exploring less invasive treatment options, underscoring the necessity of further studies to improve patient care for this condition.
We would like to express our gratitude to our patient and their family for allowing us to publish this case report.
Provenance and peer review: Unsolicited article; Externally peer reviewed.
Peer-review model: Single blind
Specialty type: Medicine, research and experimental
Country/Territory of origin: China
Peer-review report’s classification
Scientific Quality: Grade A, Grade C
Novelty: Grade A, Grade C
Creativity or Innovation: Grade A, Grade C
Scientific Significance: Grade A, Grade B
P-Reviewer: Gokce E, Türkiye; Sultana N, Bangladesh S-Editor: Zheng XM L-Editor: A P-Editor: Li X
| 1. | Altieri MS, Zheng R, Pryor AD, Heimann A, Ahn S, Telem DA. Esophageal bronchogenic cyst and review of the literature. Surg Endosc. 2015;29:3010-3015. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 9] [Cited by in F6Publishing: 11] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 2. | Coselli MP, de Ipolyi P, Bloss RS, Diaz RF, Fitzgerald JB. Bronchogenic cysts above and below the diaphragm: report of eight cases. Ann Thorac Surg. 1987;44:491-494. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 78] [Cited by in F6Publishing: 72] [Article Influence: 1.9] [Reference Citation Analysis (0)] |
| 3. | Simonetti S, Canalís E, Macías L, Carrasco MA. Clinico-pathological features of the intradiaphragmatic bronchogenic cysts: report of a case and review of the literature. Pathologica. 2018;110:116-120. [PubMed] [Cited in This Article: ] |
| 4. | Jiang C, Wang H, Chen G, Jiang G, Zhang P. Intradiaphragmatic bronchogenic cyst. Ann Thorac Surg. 2013;96:681-683. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 7] [Cited by in F6Publishing: 8] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 5. | McAdams HP, Kirejczyk WM, Rosado-de-Christenson ML, Matsumoto S. Bronchogenic cyst: imaging features with clinical and histopathologic correlation. Radiology. 2000;217:441-446. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 262] [Cited by in F6Publishing: 214] [Article Influence: 8.9] [Reference Citation Analysis (0)] |
| 6. | Govaerts K, Van Eyken P, Verswijvel G, Van der Speeten K. A bronchogenic cyst, presenting as a retroperitoneal cystic mass. Rare Tumors. 2012;4:e13. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 36] [Cited by in F6Publishing: 43] [Article Influence: 3.6] [Reference Citation Analysis (0)] |
| 7. | St-Georges R, Deslauriers J, Duranceau A, Vaillancourt R, Deschamps C, Beauchamp G, Pagé A, Brisson J. Clinical spectrum of bronchogenic cysts of the mediastinum and lung in the adult. Ann Thorac Surg. 1991;52:6-13. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 232] [Cited by in F6Publishing: 194] [Article Influence: 5.9] [Reference Citation Analysis (0)] |
| 8. | Wang SE, Tsai YF, Su CH, Shyr YM, Lee RC, Tsai WC, Li FY, Chen TH, Wu CW, Lui WY. Retroperitoneal bronchogenic cyst mimicking pancreatic cystic lesion. J Chin Med Assoc. 2006;69:538-542. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 17] [Cited by in F6Publishing: 12] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 9. | Carachi R, Azmy A. Foregut duplications. Pediatr Surg Int. 2002;18:371-374. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 55] [Cited by in F6Publishing: 56] [Article Influence: 2.5] [Reference Citation Analysis (0)] |
| 10. | Anderson MI, O'Reilly KJ, Costabile RA. Retroperitoneal bronchogenic cyst mimicking a pheochromocytoma. J Urol. 2001;166:1379-1380. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 6] [Cited by in F6Publishing: 6] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 11. | Doggett RS, Carty SE, Clarke MR. Retroperitoneal bronchogenic cyst masquerading clinically and radiologically as a phaeochromocytoma. Virchows Arch. 1997;431:73-76. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 22] [Cited by in F6Publishing: 22] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 12. | Chung JM, Jung MJ, Lee W, Choi S. Retroperitoneal bronchogenic cyst presenting as adrenal tumor in adult successfully treated with retroperitoneal laparoscopic surgery. Urology. 2009;73:442.e13-442.e15. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 18] [Cited by in F6Publishing: 26] [Article Influence: 1.6] [Reference Citation Analysis (0)] |
| 13. | Liu HS, Li SQ, Cao ZL, Zhang ZY, Ren H. Clinical features and treatment of bronchogenic cyst in adults. Chin Med Sci J. 2009;24:60-63. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 15] [Cited by in F6Publishing: 16] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 14. | Yang DM, Jung DH, Kim H, Kang JH, Kim SH, Kim JH, Hwang HY. Retroperitoneal cystic masses: CT, clinical, and pathologic findings and literature review. Radiographics. 2004;24:1353-1365. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 258] [Cited by in F6Publishing: 225] [Article Influence: 11.8] [Reference Citation Analysis (0)] |
| 15. | Lim LL, Ho KY, Goh PM. Preoperative diagnosis of a paraesophageal bronchogenic cyst using endosonography. Ann Thorac Surg. 2002;73:633-635. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 30] [Cited by in F6Publishing: 31] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 16. | He WT, Deng JY, Liang H, Xiao JY, Cao FL. Bronchogenic cyst of the stomach: A case report. World J Clin Cases. 2020;8:1525-1531. [PubMed] [DOI] [Cited in This Article: ] [Cited by in CrossRef: 5] [Cited by in F6Publishing: 5] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 17. | Wang M, He X, Qiu X, Tian C, Li J, Lv M. Retroperitoneal bronchogenic cyst resembling an adrenal tumor with high levels of serum carbohydrate antigen 19-9: A case report. Medicine (Baltimore). 2017;96:e7678. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 11] [Cited by in F6Publishing: 11] [Article Influence: 1.6] [Reference Citation Analysis (0)] |
| 18. | Miller RF, Graub M, Pashuck ET. Bronchogenic cysts; anomalies resulting from maldevelopment of the primitive foregut and midgut. Am J Roentgenol Radium Ther Nucl Med. 1953;70:771-785. [PubMed] [Cited in This Article: ] |
| 19. | Tokuda N, Naito S, Uozumi J, Shimura H, Takayanagi R, Kumazawa J. A retroperitoneal bronchogenic cyst treated with laparoscopic surgery. J Urol. 1997;157:619. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 2] [Cited by in F6Publishing: 2] [Article Influence: 0.1] [Reference Citation Analysis (0)] |
| 20. | Liang MK, Yee HT, Song JW, Marks JL. Subdiaphragmatic bronchogenic cysts: a comprehensive review of the literature. Am Surg. 2005;71:1034-1041. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 39] [Cited by in F6Publishing: 41] [Article Influence: 10.3] [Reference Citation Analysis (0)] |
| 21. | Cetinkurşun S, Oztürk H, Celasun B, Sakarya MT, Sürer I. Isolate abdominal bronchogenic cyst: a case report. Eur J Pediatr Surg. 1997;7:103-105. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 8] [Cited by in F6Publishing: 8] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 22. | Yuan K, Shu M, Ma Y, Feng W, Ye J, Yuan Y. Ectopic bronchogenic cyst in the retroperitoneal region: a case report and literature review of adult patients. BMC Surg. 2021;21:347. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 1] [Cited by in F6Publishing: 7] [Article Influence: 2.3] [Reference Citation Analysis (0)] |
| 23. | Yamamoto E, Nakayama H, Ozaki N, Kitamura Y, Funatsuka M, Ueda M, Chikugo K, Hirata A, Kurashina A, Kuratsuka H, Nakagawa M, Nagaoka S. Laparoscopically resected foregut cyst adjacent to the right adrenal gland. Diagn Ther Endosc. 1998;5:53-56. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 2] [Cited by in F6Publishing: 4] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 24. | McCrystal DJ, Borzi PA. Retroperitoneoscopic resection of retroperitoneal bronchogenic cysts. Pediatr Surg Int. 2002;18:375-377. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 15] [Cited by in F6Publishing: 16] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 25. | Hedayati N, Cai DX, McHenry CR. Subdiaphragmatic bronchogenic cyst masquerading as an "adrenal incidentaloma". J Gastrointest Surg. 2003;7:802-804. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 23] [Cited by in F6Publishing: 24] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 26. | Ishikawa T, Kawabata G, Okada H, Arakawa S, Kamidono S, Fujisawa M. Retroperitoneal bronchogenic cyst managed with retroperitoneoscopic surgery. J Urol. 2003;169:1078-1079. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 9] [Cited by in F6Publishing: 9] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 27. | Ishizuka O, Misawa K, Nakazawa M, Nishizawa O. A retroperitoneal bronchogenic cyst: laparoscopic treatment. Urol Int. 2004;72:269-270. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 9] [Cited by in F6Publishing: 11] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 28. | Terry NE, Senkowski CK, Check W, Brower ST. Retroperitoneal foregut duplication cyst presenting as an adrenal mass. Am Surg. 2007;73:89-92. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 13] [Cited by in F6Publishing: 14] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 29. | Chu PY, Hwang TI, Teng TH, Lee CC. A retroperitoneal bronchogenic cyst successfully treated by laparoscopic surgery. Ann Saudi Med. 2007;27:199-200. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 8] [Cited by in F6Publishing: 10] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 30. | Minei S, Igarashi T, Hirano D. A case of retroperitoneal bronchogenic cyst treated by laparoscopic surgery. Hinyokika Kiyo. 2007;53:171-174. [PubMed] [Cited in This Article: ] |
| 31. | Roma A, Varsegi M, Magi-Galluzzi C, Ulbright T, Zhou M. The distinction of bronchogenic cyst from metastatic testicular teratoma: a light microscopic and immunohistochemical study. Am J Clin Pathol. 2008;130:265-273. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 12] [Cited by in F6Publishing: 7] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 32. | Obando J, Merkle E, Bean SM. A retroperitoneal bronchogenic cyst. Clin Gastroenterol Hepatol. 2009;7:A24-Ae1. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 8] [Cited by in F6Publishing: 8] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 33. | El Youssef R, Fleseriu M, Sheppard BC. Adrenal and pancreatic presentation of subdiaphragmatic retroperitoneal bronchogenic cysts. Arch Surg. 2010;145:302-304. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 9] [Cited by in F6Publishing: 11] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 34. | Inaba K, Sakurai Y, Umeki Y, Kanaya S, Komori Y, Uyama I. Laparoscopic excision of subdiaphragmatic bronchogenic cyst occurring in the retroperitoneum: report of a case. Surg Laparosc Endosc Percutan Tech. 2010;20:e199-e203. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 7] [Cited by in F6Publishing: 7] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 35. | Díaz Nieto R, Naranjo Torres A, Gómez Alvarez M, Ruiz Rabelo JF, Pérez Manrique MC, Ciria Bru R, Valverde Martínez A, Roldán de la Rúa J, Alonso Gómez J, Rufián Peña S. Intraabdominal bronchogenic cyst. J Gastrointest Surg. 2010;14:756-758. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 25] [Cited by in F6Publishing: 30] [Article Influence: 2.1] [Reference Citation Analysis (0)] |
| 36. | Alguraan Z, Agcaoglu O, El-Hayek K, Hamrahian AH, Siperstein A, Berber E. Retroperitoneal masses mimicking adrenal tumors. Endocr Pract. 2012;18:335-341. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 6] [Cited by in F6Publishing: 7] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 37. | O'Neal PB, Moore FD, Gawande A, Cho NL, King EE, Moalem J, Ruan D. Bronchogenic cyst masquerading as an adrenal tumor: a case of mistaken identity. Endocr Pract. 2012;18:e102-e105. [PubMed] [DOI] [Cited in This Article: ] |
| 38. | Jannasch O, Büschel P, Wodner C, Seidensticker M, Kuhn R, Lippert H, Mroczkowski P. Retroperitoneoscopic and laparoscopic removal of periadrenally located bronchogenic cysts--a systematic review. Pol Przegl Chir. 2013;85:706-713. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 3] [Cited by in F6Publishing: 6] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 39. | Cai Y, Guo Z, Cai Q, Dai S, Gao W, Niu Y, Li G, Zhang Y. Bronchogenic cysts in retroperitoneal region. Abdom Imaging. 2013;38:211-214. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 12] [Cited by in F6Publishing: 10] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 40. | Runge T, Blank A, Schäfer SC, Candinas D, Gloor B, Angst E. A retroperitoneal bronchogenic cyst mimicking a pancreatic or adrenal mass. Case Rep Gastroenterol. 2013;7:428-432. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 16] [Cited by in F6Publishing: 19] [Article Influence: 1.7] [Reference Citation Analysis (0)] |
| 41. | Castro R, Oliveira MI, Fernandes T, Madureira AJ. Retroperitoneal bronchogenic cyst: MRI findings. Case Rep Radiol. 2013;2013:853795. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 4] [Cited by in F6Publishing: 7] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 42. | Dong B, Zhou H, Zhang J, Wang Y, Fu Y. Diagnosis and treatment of retroperitoneal bronchogenic cysts: A case report. Oncol Lett. 2014;7:2157-2159. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 11] [Cited by in F6Publishing: 14] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 43. | Cao DH, Zheng S, Lv X, Yin R, Liu LR, Yang L, Huang Y, Wei Q. Multilocular bronchogenic cyst of the bilateral adrenal: report of a rare case and review of literature. Int J Clin Exp Pathol. 2014;7:3418-3422. [PubMed] [Cited in This Article: ] |
| 44. | Terasaka T, Otsuka F, Ogura-Ochi K, Miyoshi T, Inagaki K, Kobayashi Y, Nasu Y, Makino H. Retroperitoneal bronchogenic cyst: a rare incidentaloma discovered in a juvenile hypertensive patient. Hypertens Res. 2014;37:595-597. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 4] [Cited by in F6Publishing: 6] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 45. | Zhang D, Zhang Y, Liu X, Zhu J, Feng C, Yang C, Wu S, Liu J, Hua Y, Liu F, Zhang N, He D, Lin T, Wei G. Challenge in preoperative diagnosis of retroperitoneal mucinous cyst in a pediatric patient. Int J Clin Exp Med. 2015;8:19540-19547. [PubMed] [Cited in This Article: ] |
| 46. | Trehan M, Singla S, Singh J, Garg N, Mahajan A. A Rare Case of Intra- Abdominal Bronchogenic Cyst- A Case Report. J Clin Diagn Res. 2015;9:PD03-PD04. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 5] [Cited by in F6Publishing: 8] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 47. | Jiang X, Zeng H, Gong J, Huang R. Unusual uptake of radioiodine in a retroperitoneal bronchogenic cyst in a patient with thyroid carcinoma. Clin Nucl Med. 2015;40:435-436. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 9] [Cited by in F6Publishing: 11] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 48. | Bulut G, Bulut MD, Bahadır I, Kotan Ç. Bronchogenic cyst mimicking an adrenal mass in the retroperitoneal region: report of a rare case. Indian J Pathol Microbiol. 2015;58:96-98. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 1] [Cited by in F6Publishing: 3] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 49. | Yoon YR, Choi J, Lee SM, Kim YJ, Cho HD, Lee JW, Jeon YS. Retroperitoneal Bronchogenic Cyst Presenting Paraadrenal Tumor Incidentally Detected by (18)F-FDG PET/CT. Nucl Med Mol Imaging. 2015;49:69-72. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 11] [Cited by in F6Publishing: 9] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 50. | Liu Q, Gao Y, Zhao Z, Zhao G, Liu R, Lau WY. Robotic resection of benign nonadrenal retroperitoneal tumors: A consecutive case series. Int J Surg. 2018;55:188-192. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 8] [Cited by in F6Publishing: 8] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 51. | Bolton JW, Shahian DM. Asymptomatic bronchogenic cysts: what is the best management? Ann Thorac Surg. 1992;53:1134-1137. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 85] [Cited by in F6Publishing: 90] [Article Influence: 2.8] [Reference Citation Analysis (0)] |
| 52. | Sinha V, Nandi P, Shankar M, Sardana N. Retroperitoneal Bronchogenic Cyst: A Rare Case Study. Cureus. 2020;12:e10421. [PubMed] [DOI] [Cited in This Article: ] [Cited by in F6Publishing: 1] [Reference Citation Analysis (0)] |
| 53. | Wen Y, Chen W, Chen J, He X. Retroperitoneal bronchogenic cyst resembling an adrenal tumor: two case reports and literature review. J Int Med Res. 2020;48:300060520925673. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 5] [Cited by in F6Publishing: 12] [Article Influence: 4.0] [Reference Citation Analysis (0)] |
| 54. | Qingyu J, Xiaolong L, Ruohan Z, Licong M, Zhichao T, Qingwei C, Yuan W, Ying Z. Computed tomography helps pre-operative evaluation before laparoscopic resection of retroperitoneal bronchogenic cyst: A case report. J Minim Access Surg. 2021;17:95-97. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 2] [Cited by in F6Publishing: 4] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 55. | Wu LD, Wen K, Cheng ZR, Alwalid O, Han P. Retroperitoneal bronchogenic cyst in suprarenal region treated by laparoscopic resection: A case report. World J Clin Cases. 2021;9:7245-7250. [PubMed] [DOI] [Cited in This Article: ] [Cited by in CrossRef: 3] [Cited by in F6Publishing: 3] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 56. | Cowan S, Gunawardene A, Davenport E. Retroperitoneal bronchogenic cyst mistaken as an adrenal adenoma. ANZ J Surg. 2021;91:E526-E527. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 2] [Cited by in F6Publishing: 6] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 57. | Tadokoro T, Misumi T, Itamoto T, Nakahara H, Matsugu Y, Ikeda S, Oshita A, Hotta R, Miguchi M, Chogahara I, Nishikawa S, Hiroi S, Nishisaka T. Retroperitoneal Bronchogenic Cyst Resected by Single-Incision Laparoscopic Surgery in an Adolescent Female: A Case Report. Asian J Endosc Surg. 2022;15:206-210. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 3] [Cited by in F6Publishing: 3] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 58. | Hu BY, Yu H, Shen J. A retroperitoneal bronchogenic cyst clinically mimicking an adrenal mass: three case reports and a literature review. J Int Med Res. 2022;50:3000605211072664. [PubMed] [DOI] [Cited in This Article: ] [Cited by in F6Publishing: 2] [Reference Citation Analysis (0)] |